New Technology Helps Gill Heart Institute Physicians Unmask Artifacts Left By Implantable Cardiac Devices
LEXINGTON, Ky. (July 25, 2014) -- Most people hear the word "artifact" and think of amazing items found by archeologists at a dig -- objects that shed light on bygone cultures.
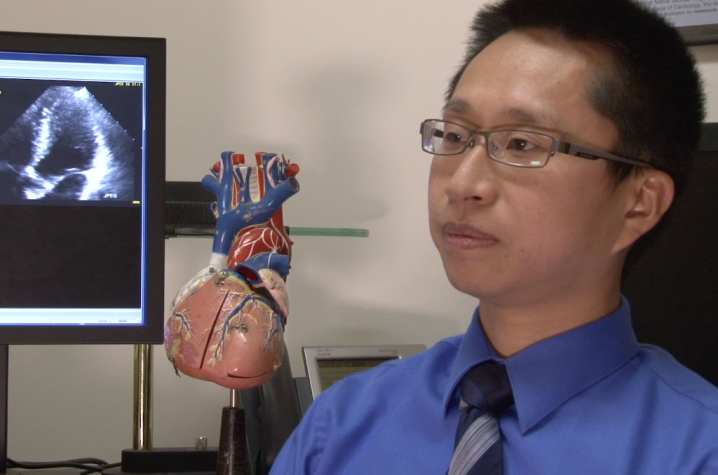
For Dr. Vincent Sorrell, and his colleagues on the Gill Heart Institute's Advanced Cardiovascular Imaging team, the thought of artifacts means a challenge but one they have worked to overcome.
"In the imaging world, an artifact corrupts our ability to see and makes it harder, if not impossible, to diagnose a patient properly," explains Sorrell. "And in the world of cardiac imaging, artifacts make a challenging job even more challenging."
Magnetic Resonance Imaging (MRI) is a unique diagnostic tool that, unlike CAT scans or X-rays, doesn't require the use of radiation or contrast agents to develop an image. Its relative safety and level of visual detail have made it a popular option for the diagnosis of disease. However, MRI was designed to capture still images -- of the brain, for example. And so special expertise is required when physicians use MRI to look at a beating heart.
"It's a carefully choreographed process," says Dr. Steve Leung, associate director for Advanced Cardiovascular Imaging at the Gill and, according to Sorrell, "the brains behind the operation."
"With cardiac MRI, we have to time our pictures in concert with the patient's heartbeat and breathing in order to get interpretable images. A lot of effort goes into getting good pictures on a moving target. So when there are factors that add artifacts to an image, it's that much more difficult to make a diagnosis."
The major culprits for artifacts in cardiac imaging are implantable cardiac devices (ICDs) such as pacemakers or defibrillators. The metal in devices like these distort the magnetic field that creates an MRI image and can render the data useless to diagnosticians.
"Most MRI centers won't scan patients with ICDs at all because of the theoretical risk involved in using a magnetic field near an object, such as a pacemaker, that has metal parts," Leung says. "Extensive research has demonstrated that, with the proper precautions and expertise in place, we can, in fact, perform MRIs on patients with ICDs. But now we have a new hurdle, and that is the ability to diagnose patients when artifacts from an ICD interfere."
Out of this conundrum was born a search for a way around the problem. And as the team explored options, they zeroed in on changes to the sequencing -- software that, in essence, tells the MRI equipment what to do and when.
"UK is unique in that we are not an island," Leung said. "We are clinicians, but there are also physicists, software engineers, and biomedical engineers, all within walking distance of one another. And so we have this incredible talent pool that has allowed us to obtain technology that almost nobody else has, so that patients with ICDs can have equal access to quality cardiac MRI."
Networking with colleagues in California, the team was able to access new sequencing software that "unmasks" the tissue surrounding an ICD.
"The very first time we used this new sequencing technique, we found a scar indicative of myocarditis, or inflammation of the heart muscle, that had been masked by the artifact created by the patient's ICD," says Leung. "It was actually pretty impressive."
According to Sorrell, this advance in imaging technology is likely to have significant impact on patients with heart problems and ICDs.
"MRI is available everywhere, but the expertise required for cardiac MRI, combined with the technology that makes us able to read MRI in patients with ICDs, that's a really small subset of medical centers who are capable of performing this technique. And now Gill has this newer technology that makes it even more precise, and we're just one of a handful in the U.S.," Sorrell says.
"I think that's why we get referrals from multiple states, from way outside the region, because people realize that what we do here at the Gill is unique."
This and the many other resources at the Gill Heart Institute are meaningful for Kentucky, where heart disease and stroke account for more than a third of all deaths annually.
"For the last 50 years or so, we've been very good at calculating the heart's pumping efficiency -- called ejection fraction -- as a means of evaluating heart disease and heart failure," Sorrell says. "But the heart is much more complex than its overall end product efficiency. Advances in imaging techniques are beginning to reveal the complex nature of the fibers that make up heart muscle, and how those fibers align and work in perfect synchrony to create a healthy, efficient heart beat."
"Being able to understand a disease at its early stage, before it starts to change the efficacy of that ejection fraction, that's going to be the way we start to identify early forms of treatment to prevent heart failure. Not just treat heart failure, but catch it before it's there."