In 1874, a doctor whose name seems to have been lost to history presented a necrometer to the Paris Academy of Medicine. Such machines—intended to determine whether a body was living or dead—were in high demand at the turn of the century. A literary tradition that includes Edgar Allan Poe stories such as “The Cask of Amontillado” as well as new medical advancements like artificial respiration contributed to popular anxieties about the nature of death: How can we be sure that a body that looks dead actually is dead? (This dilemma was also the origin of the safety coffin and many other technologies for those afraid of being buried alive.) The necrometer, with its quantitative scale of relative “vitality,” purported to answer this question.
The device presented in Paris in 1874, though, was a parody—it was nothing more than a fever thermometer with an altered scale. The “point of health”—what we know as the standard 98.6 degrees Fahrenheit—was mislabeled as 0, the indicator of death. Several of those in attendance were diagnosed as deceased. The point of the presentation: to demonstrate the absurdity of necrometry.
The stunt needled physician Édouard Séguin, who believed deeply in the thermometer’s power both as a necrometer and as a general health care tool that could be used by lay people as well as by elite physicians. The French-born Séguin, who moved to the United States in the mid-1800s, was one of the primary proponents of thermometry in American medicine, and the thermometer that had been used in the Paris ruse was one of his own design. In books, at meetings of physicians, and in popular magazines, Séguin proposed a variety of thermometers and thermoscopes for different users and purposes. Séguin, who was most famous for his work treating mentally disabled children, was also an advocate for use of the metric system in America; he believed deeply in the power of quantification in medicine and science. Despite the joke played at the Paris Academy of Medicine, Séguin was convinced that technology would eventually be able to provide the certain diagnosis of death.
Séguin also believed that such a powerful tool should not rest only in the hands of physicians. Despite resistance from many of his colleagues in the medical community, he wrote extensively about how mothers and other family members should learn to use thermometers to take and record the temperatures of their loved ones. He believed that this ability, which would be enhanced by the gentleness and knowledge of a mother’s touch, would enable mothers to keep better watch for signs of approaching illness. Just as today we keep track of changes in our sleep, blood pressure, and diet in order to ward off health problems later, a vigilant mother would be able to notice immediately when her child’s temperature indicated danger, and she could contact a physician right away.
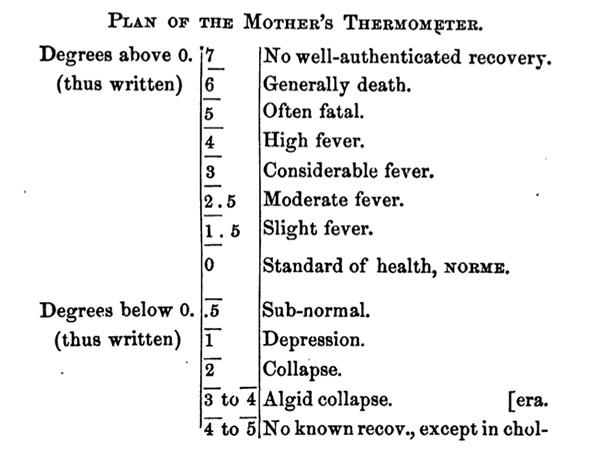
To this end, Séguin designed a targeted “mother’s thermometer” that he promoted in his popular manual Family Thermometry. Instead of being labeled according to a Fahrenheit or Celsius scale, it would follow the model of the necrometer, with a simplified “Scale of Vitality.” The scale, which was reproduced in the manual, ran both up and down from 0, which indicated a “standard of health,” to 5, which was labeled “often fatal.” For the most dire of circumstances, its scale topped out at a high temperature of 7, which indicated “no well-authenticated recovery.” Lower temperatures below 0 were also problematic, indicating “depression” or “collapse.”
Courtesy of Deanna Day
Despite producing and promoting his inventions in his manual, in professional literature, and to an audience of physicians, neither Séguin’s mother’s thermometer nor his necrometer was ever widely used. Séguin recognized that thermometry and quantitative symptom tracking were becoming central components of modern medicine, but he did not fully understand why. Thermometers became a solution not only to a diagnostic problem but also to a labor problem.
Thermometers are useful because they reduce a patient’s bodily experience to a discrete measurement, one that is not only clear but also comparable to all other temperature measurements. They are not only diagnostic technologies that translate a component of a living body into a form that an individual can understand but also communications technologies that produce information in a form communicable to other people. The data produced by a thermometer can only be transmitted to different people if they interpret it using a shared system. For thermometers, this shared system was the Fahrenheit or Celsius scale.
Many physicians objected to the introduction of the thermometer in medicine because they perceived it to be a threat to their expertise. If a simple tool made of mercury and glass had the power to indicate whether someone was healthy or sick, or alive or dead, then physicians were concerned that they would lose both their cultural authority and their livelihoods.
Instead, physicians were able to realign the hierarchy of medical labor such that it included lay people along with physicians while maintaining the physician’s position as the head. With physicians, nurses, mothers, and even patients all able to detect and record temperature on the same scale, each of their individual temperature readings were comparable with one another and, just as importantly, were in the same “language” of temperature in which the physician was already fluent. The temperature scale enabled a whole network of people to contribute to a single temperature chart and, therefore, to the collection of information on which a physician would base his opinion. The physician, then, was able to delegate the authority for collecting temperature data while maintaining the authority to interpret temperature data.
Séguin believed so strongly in the thermometer’s diagnostic power to read the body that he overlooked, and even eliminated in his own designs, the characteristic that has made them most useful to modern medicine: the standardized Fahrenheit or Celsius scale that made temperatures taken by different people comparable with one another. The thermometer was the first scientific medical instrument to enroll such a large network of nonprofessional workers into the new medical system, creating a model for distributed care that continues into the 21st century as we track our own temperatures, blood pressure, and calorie intakes.
When we create new technologies and new ways of using them, we rarely understand what their ultimate value will be. What begins as an immediate solution to present problems can have unintended consequences that structure industries and lives. And even when inventions seem laughable—like the necrometer—they might eventually transform into technologies with lasting power.
Although the necrometer ended up nothing more than a joke and a failure, the medical labor system that thermometry and Séguin’s teaching made possible has made all of us constant monitors of our bodily metrics. We know we are alive, and we know it differently.
