A

IN THIS ISSUE
From










From








A new ERA for aged care
Landmark aged care campaign wins prestigious award
a wrap!
On the road to reform 17 Aged care workers get a pay rise 19 Nurture your leaders 21 Investing in nursing to build a resilient, highly qualified workforce 23 Rounding out retirement living reform 25
The fatal impulse: Why data and automation need human systems 27
The Home Care Careers Portal launches in VIC/TAS 28
Overcoming the aged care skills shortage in NSW/ACT 30
More home care workers for SA/NT 33 The pros and cons of the new Support at Home Program 35
New early indicator of dementia identified 37 New guide on non-medication treatments for BPSD in dementia 41 Get moving 42 Young and old together 43
Addressing hearing loss in aged care settings 47 Dining with dignity 49 IPC 101 50
All-Australian hygiene innovation 51
CULTURE
Let’s end ageism 53 Not just one hand clapping 54
“They speak my language” 56
Older migrants need housing support 58 The silent suffering of loneliness 61 Age no barrier as teens connect with seniors to break down digital divide 62
Transitioning younger people out of residential aged care 63
Shifting the focus 65
Younger home care workers are a natural solution 67
Humans of Aged Care 68

Rising above the floodwaters 69
Why a WFM solution should be your go-to 71 No workers to hire or can’t we find them? 73
Training to keep personal care workers safe 74 Build your workforce into more than a pulse 77
Getting dementia training right 79
A new way to say thanks to your staff 81
Recognising talent 83
New governance requirements 84 Why good governance is so important 87
Safeguarding care 88
A transparent approach to asset maintenance 90
Contract complexity dampens retirement village appeal 92
Inheritance conversations: ‘gifts’ in and of themselves 93
Winning innovators 94
BrainTrack and early dementia diagnosis 96
Defying the odds with technology 97
The power of RTLS technology in residential aged care 99
The right technology solutions to meet standards 100
The challenge of our time 101
Step up your incident reporting 102
How to support mental health in the circle of care 103
What to look for in a digital transformation partner 104
A new type of ‘care community’? 106
Shifting the paradigm on institutional living 108
A foreground architecture design for Australian Unity 109
A home away from home at the ECH Care Hotel 110
Supporting inclusive environments 112
What’s new 114
Welcome to our summer 2022 issue of Aged Care Today – the magazine of Aged & Community Care Providers Association (ACCPA).
In this issue, we hear about policy directions for 2023, training offerings and workforce strategies.
We explore what it means to support Aboriginal and Torres Strait Islander Elders, as well as people from culturally and linguistically diverse backgrounds. We learn about new initiatives in relation to dementia, and we continue the discussion about better ways to live in residential care – from food, hearing checks and upgraded hygiene to building design.
There is a wealth of information in articles about good governance and the value of technological innovations – and so much more.
As always, this issue couldn’t have happened without our wonderful contributors and the many incredible initiatives happening in aged care.
Linda Baraciolli, Editorby the Association for statements of fact or opinions expressed in signed contributions. Aged Care Today may be copied in whole or distributed among an organisation’s staff. No part of Aged Care Today may be reproduced in any other form without written permission from the article’s author.
shot: Salvatore Virzi
Aged Care
is the regular publication of Aged
Unsolicited
are welcome but ACCPA reserves the right to edit, abridge, alter or reject material. Opinions expressed in Aged Care Today are not necessarily those of ACCPA and no responsibility is accepted
Grace Pennisi, Group Coordinator at Co.As.It Casa Serena
Brisbane. Salvatore says he enjoys going to the social group and being able to connect with people who speak Italian.






As we head into summer I hope many of you will have the chance to take a restful break. After last summer, we could all do with a quiet holiday!
It has been an incredibly busy few months with the new Labor Government taking a new approach to the aged care reforms emanating from the Royal Commission into Aged Care Quality and Safety final report. Our policy team has been working hard to keep up with the legislation and consultation papers being released.
We have been finalising the establishment of the new Aged & Community Care Providers Association (ACCPA) and held our inaugural National Conference in Adelaide in October which was a tremendous success.
A highlight for me was the launch with our new CEO Tom Symondson of ACCPA’s new Members’ Charter. The Members’ Charter enshrines the values of Australia’s largest aged care provider organisation. These values underpin our vision which is to enhance the wellbeing of older Australians through a high performing, trusted and sustainable aged care sector.
Our commitment to our Members is to lead, advocate and provide support, advice and guidance, so that the older people we care for and support can live their best lives.
This is our goal. This informs and drives all that we do.
The establishment of our Members’ Charter represents an important milestone for our sector and for the standing of ACCPA.
Closer to home, we have been finalising ACCPA’s establishment and developing our goals for the coming year. It was a thrill for me to deliver the welcome address to the ACCPA National Conference where so many of our Members and Partners were able to gather together, some for the first time since 2019.
As a first gathering under the ACCPA banner, there was a sense of a groundswell of support for our new unified voice for aged care. We welcomed many distinguished guests and speakers including Minister for Aged Care Anika Wells MP.
The interest in the wide variety of topics in the 80 plenary sessions and the myriad fishbowl and breakout sessions was exceptional as delegates found there was plenty to learn and talk about. This is something of a hallmark of our industry: the eagerness to learn, collaborate and find ways of doing things better.
As we move into the new year, there is much work ahead of the team at ACCPA and for the sector generally. The Fair Work Commission work value decision, for example, and the federal government commitment to fully fund the outcome provides the potential for a fresh and positive start to 2023.
We are looking forward to establishing the bedrock of a genuine partnership for aged care reform with the government to which an improvement in the pay of the aged care workforce is a crucial element.
While aged care providers must remain vigilant and do all that they can to protect older vulnerable people against COVID-19, we can dare to hope that the most challenging days of the pandemic are now behind us.
If that is the case, then we can work fully with the government to see crucial reforms including those to residential care implemented during the year and ensure our Members have input in the shape of our new home and community care program.
All of this means that with the new government the pace of reform has quickened and the demands on our sector may seem heavier but we must not lose sight of the goals, as identified by the Royal Commission, to improve the quality of care for older people.
We are seeking a respectful relationship with the government, one that listens to the voices of those who work in our sector. The hallmarks of this relationship must be Excellence, Respect and Accountability – a new ERA for aged care.
ACCPA will lead with a fresh approach, one that is assertive, collaborative and effective.
Dr Graeme Blackman AO FTSE FAICD, Chairman, Aged & Community Care Providers Association www.accpa.asn.au

Our aged services industry must be founded on pillars of Excellence, Respect and Accountability

Welcome to the summer 2022 edition of Aged Care Today. As this is my first column as CEO of ACCPA, I want to take the opportunity to share with you some reflections on my first month or two with the organisation.

It was wonderful to meet so many of our Members at our inaugural ACCPA National Conference in Adelaide in October. I am told it was the largest ever gathering in Australia of aged care providers and those involved in our industry, with more than 1,800 people present. It was a tremendous success and I thank those of you who attended for taking part. I have had some incredible feedback about the event from all over the sector as I’ve travelled across the country to meet Members.
My background in public health and particularly spending the pandemic representing public and community health providers in the world’s most locked-down state, means that I am all too familiar with the complexity and challenges that have been faced by so many of our Members over the past few years. Yet you are still working, turning up every day, to support older people.
Since September there have been some positive gains for our sector and for broader aged care reform. The parliament passed legislation to provide extra care minutes and additional nursing support for aged care residents, and the government included funding for these important measures in its October budget.
We have also seen the start of AN-ACC, the introduction of Star Ratings for aged care homes based on client experience interviews among other things, consultation on new quality indicators, and the release of a discussion paper on the new in-home care program scheduled for 2024.
And yet the headwinds are still significant. Wherever I have travelled, while Members have shown me fantastic examples of innovation and high-quality services for older people, they have also described a situation of constant financial pressure and workforce shortages.
The Albanese Government has accelerated the pace of reform, much of which is welcome, but there is no escaping the reality that our sector is exhausted by years of the pandemic and weighted down by years of underfunding, which will take significant time to resolve.
While workforce remains a significant challenge, we welcomed the recent interim decision by the Fair Work Commission to increase the minimum rates of direct care staff by 15 per cent. This is a positive first step in addressing our workforce challenges, although we still await a decision on other staff such as cooks, kitchen staff, maintenance and administrative workers, as well as a final decision on whether the increase will move to the 25 per cent requested by the Health Services Union and Australian Nursing and Midwifery Federation. We are now focused on working with government on the implementation of this decision to ensure they are able to fulfil their promise to fully fund its costs.
As CEO, I want to work on your behalf to rebuild public trust in aged care in Australia. We need to change the focus from constant negative stories which serve only to demoralise our hard-working staff and reduce public confidence in our sector.
While we must not shy away from facing our failings, nor seek to avoid accountability when things go wrong, punitive punishments and ritual humiliation serve no useful purpose, least of all to the older people we are here to serve. Instead, where things go wrong, we have to learn from them, and move forward.
We need to embrace a focus on continuous improvement –our sector is well aware of this, but it must be a joint effort, enabled and re-enforced by government and the regulator. And we need to focus on the good news stories of highquality care and innovation – enabling providers to learn from each other and improve outcomes for older people, rather than living in fear of making even the smallest errors and the public humiliation and condemnation that often comes with them. That is the only way that positive change will happen.
That means building partnerships with government, unions, consumer advocates and others who are part of our industry so that we can achieve reforms that truly raise the quality of care for the people who receive our support and services. Because ultimately, we are in this together, and it truly is up to us.
Tom Symondson, CEO, Aged & Community Care Providers Association www.accpa.asn.au
As reform takes shape, rebuilding public confidence is a must


The Albanese Government is committed to stopping the neglect in the aged care sector – putting security, dignity and quality back into the aged care system for workers and older Australians.

We have wasted no time getting to work to reform aged care, acting on the recommendations of a damning Royal Commission report that found systemic problems that have failed a generation of hard-working and deserving Australians, and the workers who support them.
The people who look after our most vulnerable have been undervalued for too long.
The 15 per cent interim pay increase for workers in direct care roles, announced by the Fair Work Commission in November, is a first step in properly valuing the important and difficult work our aged care staff do.
We said we would back a wage increase for aged care workers – and we did.
We said we would fund any increase to award wages – and we will.
Our commitment to aged care reform has been backed up with a $3.9 billion investment in our government’s October Budget. This Budget takes the first steps to deliver the reforms that the system so badly needs.
We’re delivering on our promise to increase the number of care minutes residents receive – increasing to an average of 215 minutes from 1 October 2024, with 44 of those minutes delivered by a registered nurse.
From 1 July 2023, all aged care homes must have a registered nurse on site 24 hours a day, seven days a week. This legislation passed Parliament in October and it was an incredible milestone for our government and for older Australians.
The new laws require regular financial and operational reporting from providers to show how much is being spent on care, nursing, food, maintenance, cleaning and administration.
They also ban exit fees and cap administration and management charges in the Home Care Packages Program.
We’re supporting providers to adjust to the new Australian National Aged Care Classification funding model, to implement the increased care minutes and deliver enhanced reporting requirements.
And while laws and regulation are important, we know that without a strong, professional and valued workforce there is no aged care sector. If we don’t start paying aged care workers properly, we won’t be able to attract and retain enough staff to care for our loved ones as our population ages.
The work we do today will ensure a safe, sustainable system where our older Australians and aged care workforce receive the dignity and respect they deserve. I thank you all for sharing our commitment to building an aged care system that Australians can be proud of.
The Hon Mark Butler MP Minister For Health And Aged Care



Aged care has claimed the spotlight, with the Australian Aged Care Collaboration (AACC) campaign ‘It’s Time to Care About Aged Care’ acknowledged as Best External Campaign by the Association’s Forum in November 2022.
Australia has spent more than two decades trying to fix aged care. There have been more than 20 reports on how to fix the system, but successive governments have responded with piecemeal solutions, failing to create the change required.
The Royal Commission into Aged Care Quality and Safety was a watershed moment, highlighting the systemic problems in Australia’s aged care system.
During early Royal Commission hearings, politicians and media would frequently highlight failures and criticise providers. However, what was necessary was the political will, and in order to create an environment for change, the focus of the argument needed to shift.
The AACC, which comprised six aged care peak bodies –Anglicare Australia, Baptist Care Australia, Catholic Health Australia, UnitingCare Australia, Aged & Community Services Australia (ACSA) and Leading Age Services Australia (LASA) – created the ‘It’s Time to Care About Aged Care’ campaign, which succeeded in shifting the focus to systemic policy and funding failures.
With continued activity through mainstream media and social media from February 2021 right up to the 2022 Federal Election, we successfully realised the biggest ever Government investment in aged care ($18 billion) and turned
aged care into an election issue for the first time – regularly topping election issues surveys and becoming a key element of the ALP manifesto.
While the aged care system remains under pressure, with ongoing workforce shortages and underfunding, substantial steps are now being taken towards a world class aged care system that can sustainably support the needs of older Australians.
ACCPA CEO Tom Symondson says bringing six organisations together to lead the sector and provide one strong and consistent voice, while not without its complexities, had a huge impact on the campaign’s success.
“The ‘It’s Time to Care About Aged Care’ campaign highlights the incredible motivation within our aged care sector to achieve an aged care system Australians deserve,” he said.

The campaign included the It’s Time To Care About Aged Care Report; around 40 media releases; an election scorecard that rated the different political parties in relation to their aged care policies and election promises; a user-friendly website complete with resources for aged care providers and other campaign supporters; webinars for providers to encourage local activity; and a public petition that gained almost 50,000 supporters, each of which sent an automated letter to their local MP.
The AACC was supported to run the campaign through Apollo Communications and Industrial Australia in the post Royal Commission phase, and then by Essential Media in the lead up to the Federal Election.
The impact of our campaign continues to resonate, with a recent national poll revealing that improving aged care funding was the top priority for Australians in the Federal Budget.
The new peak body Aged & Community Care Providers Association ACCPA (formed through unification of ACSA and LASA) along with other AACC members are now working with the Albanese Government to ensure the promised changes and improvements are delivered for the long term, sustainable benefit of providers, workers and the older Australians in their care.
Linda Baraciolli, Aged Care Today Editor & Communications Advisor, Aged & Community Care Providers Association www.careaboutagedcare.org.au
ACCPA’s inaugural National Conference attracted over 1,800 delegates who packed out the Adelaide Convention Centre over three days in what has been billed as Australia’s largest ever gathering of aged care providers.

From early on the first day as delegates queued to register, there was a palpable buzz throughout the centre. For many it was the first time since before the pandemic and Royal Commission they’d had a chance to catch up with colleagues. As one delegate remarked, “it was a case of exhale, breathe in, and debrief”.
The buzz didn’t end there. With more than 80 plenary sessions, a raft of breakfast and fishbowl sessions, and a Trade Hall of around 160 exhibitors champing at the bit to show their wares to delegates, the scene was set for a busy conference.

ACCPA Chairman Dr Graeme Blackman AO welcomed delegates to the inaugural ACCPA National Conference which was kept moving along by MC Anne Fulwood.
Delegates heard from Aged Care Minister Anika Wells, Opposition health spokeswoman Senator Anne Ruston and Greens aged care spokeswoman Senator Janet Rice. There were sessions from senior Department of Health and Aged Care officials on key reforms to home and community care, and residential aged care, and a speech from Aged Care Quality and Safety Commissioner Janet Anderson PSM.
A highlight of the first day was the launch by Dr Blackman and new ACCPA CEO Tom Symondson of the ACCPA Members’ Charter which sets out the goals of the new organisation. Both of them signed the charter which was then framed.
On day two, Tom Symondson gave his first speech revealing his commitment to the aged care sector and giving a glimpse of how he sees ACCPA’s future advocacy. He emphasised that older people who
receive our care and support are at the centre of everything ACCPA does.
On day three, former Morrison Government Aged Care Minister Ken Wyatt closed the conference with a heartfelt and aspirational speech about the need for reform that gives older Australians a chance to live their best lives. He appealed to all sides to look beyond divisions or factions and to see the best way forward.
Delegates could take a break from the long list of meaty topics about nearly every aspect of aged care, and take a stroll
through the Trade Hall where they could get coffee, play mini-golf or mini-basketball, and sample treats like ice cream and chocolate.
Another feature of this inaugural national conference was ‘ACCPA Alley’ which featured ACCPA staff ready to talk to delegates about membership, partnership, training, ELDAC, residential care, home and community care, and more.
Kate Hannon, Senior Media & Communications Advisor, Aged & Community Care Providers Association www.conference.accpa.asn.au

















Since the Royal Commission into Aged Care Quality and Safety handed down their Final Report: Care, Dignity and Respect in February 2021, the aged care sector has been operating in the context of aged care reform and a global pandemic.
Additionally, we have seen a change of government this year that has stalled and then catapulted a flurry of reform activities in recent months. We can further throw into the mix an array of economic and workforce challenges that, being escalated by the pandemic, are central to the progression of aged care reform.
With this in mind, it appears that we are at a critical point for building sector confidence in government leadership to navigate us through the process of reform implementation.
Many major reform activities have emerged in recent months, including:
■ consultation on developing a new approach to regulating aged care
■ consultation on a national aged care data strategy
■ commencement of residential aged care funding via the Australian National Aged Care Classification (AN-ACC) Framework
■ consultation on the new in-home aged care program to commence 1 July 2024

■ implementing the Specialist Verification Framework for My Aged Care to approve services capable to meet the targeted consumer needs
■ consultation on the revised Aged Care Quality Standards
■ commencement of the Aged Care Quality and Safety Commission capability review
■ commencement of serious incident reporting by home care services
■ commencement of strengthened provider governance arrangements
■ consultation and commencement of a code of conduct for aged care.
Further upcoming reform activity will build on this investment throughout 2023:
■ commencement of star ratings for residential aged care
■ capping of home care package administration pricing
■ progressing implementation of the decision of the Work Value Case for aged care wages
■ implementing a large-scale trial of the assessment tool and process for the new in-home aged care program
■ consultation on an alternative in-home care delivery model for Indigenous Elders
■ expansion of quality indicators for residential aged care
■ efficient pricing of residential aged care and respite care for AN-ACC based on advice from the Independent Health and Aged Care Pricing Authority.
This extensive list of reform activities, while not complete, highlights the enormity of the transformation process the aged care sector is contending with in reform implementation.
It is also important to note that reform implementation is set against a background of economic upheaval and workforce supply constraints. It is likely this combination of socio-political factors will overshadow the aged care reform implementation experience for some time, with no immediate relief in sight.
If these factors are not managed carefully, there may be deterioration of both provider and public confidence in the reform process.
ACCPA is acutely aware that to achieve a world-class aged care system, the scope of these reform activities must collectively work towards facilitating a balanced approach between improving program funding, enabling consumer choice and securing adequate workforce supply. The interaction of these three input variables is absolutely critical. We must avoid tipping this balance too far one way or another, otherwise reform implementation will suffer and with it the experiences and outcomes we seek for the future of older Australians.
While October’s Federal Budget provided opportunity for further investment in aged care reform, the commitment appears measured. We saw the economic impacts of the COVID-19 pandemic instead create an incentive to delay additional government spending in aged care, this likely being pushed back for further consideration in the next budget.
With the list of provider issues continuing to grow, including deteriorating finances, increasing recruitment and retention challenges, continued COVID-19 waves, and high numbers of complaints and incidents with adverse regulatory findings, some providers are referencing success in this sector as staying on the road to reform.
As such, strong provider governance, robust industry leadership and an attitude of perseverance from all involved will be necessary in navigating this long and winding road with its bumps, bends and hairpin turns. Just staying on the road is the immediate challenge for aged care providers, let alone our collectively arriving at the destination on time.
Troy Speirs, Senior Policy Advisor, Aged & Community Care Providers Association www.accpa.asn.au
We’ve been really pleased to have the support of Rural LAP in providing registered nurses for our aged care facility. They come with the skills and understanding of the needs of our elderly citizens.

They know that we’re here to serve the community and when Rural LAP staff come, they join in that team.

“They

Late on 4 November 2022 there was much excitement when the Full Bench of the Fair Work Commission (FWC) handed down what is the Stage 1 Decision on the Aged Care Work Value Case.
After around two years, multiple days of hearings and hundreds of pages of submissions from all the parties, the FWC has awarded an interim 15 per cent wage increase for the following classifications in three modern awards:
■ Nurse Practitioners, Registered Nurses, Enrolled Nurses, Assistants in Nursing classifications in the Nurses Award 2020
■ Personal Care Worker classifications (Grades 1 – 3) in the Aged Care Award 2010
■ Home Care Employee classifications (Levels 1 – 3) which are involved in direct care under the Social, Community, Home Care and Disability Services Industry Award 2010
While aged care providers and those employees not in the above classifications may be disappointed that not all of the classifications under these awards have been addressed in this Decision, there is still much more to come with the Work Value Case. The FWC has decided to split the matter into three stages, with the next ones still to come.
In this Stage, the FWC will consider the following:
■ the likely impact on employment costs for aged care providers in relation to the awarding of the interim increase taking into account the extent of funding support to be provided by the Commonwealth Government
■ when the interim 15% wage increase will become operative and whether it will be phased in
■ the application of specific sections of the Fair Work Act in regards to the principle of equal remuneration
■ any agreement between the parties in relation to an interim increase for Head Chefs/Cooks and Recreational Activities Officers/Lifestyle Officers.
Submissions from the parties will be invited by the FWC, and ACCPA will be making submissions on all these critical matters.
To start Stage 2, the FWC has set down a Mention to take place 22 November 2022. At the Mention, the FWC will likely schedule dates for any necessary conferences to be held and the dates for filing submissions and further evidence. It is
unlikely that we will find out on that day when the interim 15 per cent increase will become operative.
Stage 3
This Stage will have three parts to it:
■ the consideration of the work value claim for all those award classifications that will not receive the interim increase as this was not dealt with in the Stage 1 Decision
■ a determination of any further wage adjustments that are justified on work value grounds for those classification that will receive the interim 15 per cent increase (this is because not all of the material put before the FWC was considered in setting the interim increase, in particular, the FWC has not yet taken into account the impact of COVID-19 or the issues arising from understaffing on work value for those classifications)
■ a detailed consideration of the classification definitions and structures in the three awards.
The FWC will be inviting interested parties to make further submissions and to put on further evidence to address these matters. It will then consider these submissions and evidence before making a final Decision.
As can be seen in this three-stage process, there is much work still to come in the Work Value Case. ACCPA is committed to continuing to fully participate in this highly significant case for the aged services industry to ensure that the voice of aged care providers is heard.
Claire Bailey, Workplace Relations Manager, Aged & Community Care Providers Association www.accpa.asn.au

Great leaders aren’t just born, most of them learn from other great leaders, and with the humility of an effective leader, they will happily accept training to sharpen their skills and abilities.
Leadership in aged care is a learned skillset honed during the career journey, often in a variety of roles and settings. But leaders need to be nurtured, in order to thrive.
“Google great leaders and you might get some questionable results, but we instinctively know when we are in the presence of an empowering leader and many of us count these experiences as career-defining,” says Tegan Roberts, Industry and Workforce Development Product Development Manager at Aged & Community Care Providers Association (ACCPA).
“Great leadership is best nurtured into full expression in environments that foster, promote and invest in leadership development.”
It’s not enough to appoint someone to a leadership position and hope that they will flourish. With all the stressors, demands and challenges placed upon them, they need the right support to thrive in their day-to-day tasks, as well as having the capacity to survive the tough times, and bring their team with them.
It goes without saying that leadership training is a must, but not just any training, it needs to be the right fit for what’s required in the aged services industry. To meet the needs of the sector, ACCPA has developed a suite of professional development opportunities customised for specific roles in aged care – giving your leaders and managers the tools and insights to sustain them in times of reform and change.
ACCPA is delighted to offer the Comprehensive Leadership Program, which commences on 28 February 2023. Designed for Level 2 and 3 leadership positions in aged care, it is ideal for those transitioning to a leadership role or those who would like to refresh their skills.
The program enables participants to take a deep dive over six months of learning with online coursework and one-toone coaching sessions. Each module dovetails into the next, building confidence and challenging leaders to stretch and apply new knowledge to their workplace roles.
Learning begins with a self-assessment tool, the CILCA 360, to help leaders better understand themselves, their leadership style, and their capabilities. This is followed by four separate modules designed to
develop skills, knowledge, and capabilities, to create confident, purposeful, and effective aged services leaders.
During the program, participants engage in an online Community of Practice, which continues post-program for Alumni, and is fantastic way to build the all-important networks that we all need.
The program is delivered by Cheryl Edwards, a well-respected ACCPA specialist, who is a Registered Nurse and has over 36 years of experience in residential aged care management. She has worked for smaller, larger and not-for-profit providers, in both corporate and operational roles and in leadership development. Cheryl holds qualifications in management, work, health & safety, and is a workplace trainer and assessor. And just as important, Cheryl has a big heart for aged care.
“Aged care staff are unsung heroes and I’m incredibly proud of them. We have a lot of talented, caring and highly skilled people in our industry, and it’s vital that we support them to help retain them in the aged care workforce,” said Cheryl.

“The participants in our course have found the training and the ongoing networking support really worthwhile, and I encourage organisations to consider it for their team leaders and managers.”
Registrations for the Comprehensive Leadership Program are now open, with Early Bird registration offering the CILCA 360 tool at a reduced rate, in partnership with Data Drives Insight and Human Services Skills Organisation.
Linda Baraciolli, Aged Care Today Editor & Communications Advisor, Aged & Community Care Providers Association www.accpa.asn.au/event/comprehensive-leadershipprogram/

Research strongly indicates that the key to a successful Transition to Practice Program is the provision of strong support for all stakeholders, and ACCPA’s unique Nursing Transition Program offers a supportive encouraging environment for organisations and nurses in aged and community care.
We cannot provide the best possible support or care for older Australians without the significant contribution of nurses. ACCPA coordinates the nursing programs for aged care organisations across Australia, ensuring nurses receive the required support as they enter the aged care workforce.
Our programs provide a positive experience in which nursing graduates and transitioning nurses can consolidate and further develop their knowledge, skills and competence, offering a platform for developing safe, confident and accountable professionals.
ACCPA’s role includes promoting the program to potential applicants and acting as the conduit between organisations and nurses who want to work in the sector. Our nursing team are experts in their field and are responsible for participant and organisation engagement, training, networking opportunities and inductions.
The 2022 program has attracted over 250 Graduate Registered and Enrolled Nurse participants, as well as 197 aged and community care organisation partners.
Riverview Lutheran Rest Home in South Australia partnered with ACCPA for the Nursing Transition Programs in 2022, and were delighted to be able to access professional, well trained and prepared staff.
General Services Manager Annie Payne says, “Attracting staff to the industry and workforce shortages can be very challenging, so we were thrilled to learn of this program and jumped on board immediately.
“We were then able to access nurses who were looking to work in aged care, prepared to move to our region and to benefit from the great support this program provides.
“Within a matter of days, we had secured a new RN who very quickly packed up her life, moved to our town and started with us. She is keen, eager, excited, motivated to learn and is fitting well into our team.
“This is a win-win situation for both parties and we are thrilled to be involved and thank ACCPA for this initiative. I am confident we will be involved again next year.”
Partnering aged care organisations in this program are responsible for preparing the workplace for new nurses to enter and identifying experienced Registered Nurses to mentor, guide and support their new nurses from the start to the completion of the program. On the job learning and development is critical to the success of the program, as well as attending the professional development sessions.
Sharnie Bennett, an Enrolled Nurse at AVEO in Queensland has benefited from the program and encourages others to join.

“I encourage people if they have the chance to experience working in the aged care sector, to go for it,” says Sharnie.
“Through this program, you’ll learn so many important skills, like communication, how to communicate effectively with all different types of people, and you can take it wherever you go.
“I highly recommend this program to providers as well. It will give skills to your nurses, help them to be confident and have more knowledge on how to perform better, and in future they can pass that on to any future nurses and keep building a good culture of nursing.”
The next intake for ACCPA’s Nursing Transition Programs is in February 2023. Aged care organisations across Australia can express their interest today.
Alexandra Harrison, Industry & Workforce Development Information Coordinator; Helen Li, Industry & Workforce Development Officer - Information Graduate, Aged & Community Care Providers Association www.employment.agedservicesworkforce.com.au/acttpp_ organisation/



























































As we approach the end of yet another year full of retirement living legislative reform across many states, it’s time to review the progress to date.
While we are seeing similarities starting to appear in the recommendations being presented to respective state Ministers, we are still a long way from developing a uniform set of legislation at a national level, and currently there is no legislative reform process in Tasmania, the Northern Territory or the ACT.
With asset management plans now bedded down as part of the legislative reform in NSW, we have seen the introduction of the data collection portal. On 1 September 2022, the Retirement Villages Amendment (Operators Obligations) Regulation 2022 came into force in NSW to enable the collection and publication of information regarding retirement villages.
Operators have been asked to populate the online Retirement Villages Portal at www.nsw.gov.au with information such as: contact details for the retirement village and operator; resident committee details; number of units; residency type; complaints handling processes; contract types and pricing; demographic information on residents and staff; and management and operation details. This was required by 30 September 2022.
If your information changes after being uploaded, you must update that information within 21 days of becoming aware of the change. There is also a requirement to provide annual and updated information. This must be done within one month of the end of your village financial year.
After several years of meetings through the stakeholder reference group (SRG) with Consumer Affairs Victoria
(CAV), we are reaching the pointy end of the process. On 8 October 2022, the Victorian Government released the Retirement Villages Amendment Bill 2022 Exposure Draft and the SRG met with CAV and the Minister Melissa Horne just days later, with the Amendment Bill open for consultation up until 28 October 2022.
The SRG did express its concerns at such a short time frame but it appears this was politically driven by the requirement for a ‘caretaker period’ four weeks out from the Victorian state election. We expect to meet once again with the SRG and CAV in early December after the result of the State election is known.

The Queensland Government released the final consultation document from the Housing Legislation Amendment Act (HLAA) stage 3, being the Housing Legislation Amendment Bill 2022 on 19 August 2022. Stakeholders were asked to respond by 26 August 2022.
On 27 October 2022, the Minister for Communities and Housing, Minister for Digital Economy and Minister for the Arts introduced the Bill into Parliament. The Department states that the purpose of the Draft Bill is to improve transparency, consistency and accountability in financial reporting for retirement villages. The Bill has been referred to the Community Support and Services Committee for consideration. The Parliamentary Committee has also called for submissions on the Bill.
The Retirement Villages unit from the Office of Ageing Well (OFAW) in South Australia are in the process of preparing papers for the Minister to seek approval from Cabinet to draft an amendment bill for consultation.
The Minister has indicated that he is supportive of the recommendations in
the independent report prepared by PEG Consulting and is also looking to extend some additional areas.
We anticipate that the drafting will commence by the end of 2022 after approval is given. OFAW will be conducting additional round table discussions on statutory repayment and other issues that have been identified as needing additional information and clarification from stakeholders.
OFAW plan to release the draft bill and go out for consultation in early 2023.
After four Consultation Regulatory Impact Statements (CRIS) papers published between August 2019 and June 2021, in early 2022 we arrived at a Decision Regulatory Impact Statement (DRIS) recommending amendments to the WA Retirement Villages Act 1997
There are five key areas of reform recommended:
1. information disclosure (simplifying precontractual disclosure requirements)
2. payment of exit entitlement time limits (12 months)
3. village management (targeting financial arrangements for operations and the maintenance of capital items)
4. village land (clarity about memorial requirements ensuring a resident’s interest is protected, but maintaining flexibility for operators to make changes to village land)
5. village changes (providing safeguards for residents as a result of any village changes).
We now expect a bill containing the proposed amendments to the legislation to be prepared and introduced to Parliament.
Paul
Murphy,Principal Advisor for Retirement Living & Seniors Housing, Aged & Community Care Providers Association www.accpa.asn.au





“The first rule of any technology used in a business is that automation applied to an efficient operation will magnify the efficiency. The second is that automation applied to an inefficient operation will magnify the inefficiency.” – Bill Gates
In our sector’s push towards measuring and automating everything, it’s important to remember that businesses exist to serve people, beyond this, they have no reason to be.
All tools and measurements are merely a means towards delivering better care, and in a complex sector like ours, you cannot measure complexity – there are just too many variables.
Much premium has been placed on data. Taking stock of sector discussions on data, there is a naïve view that collecting data itself will naturally lead to better decisions and processes.
This is a flawed impulse based on a simplification. Data is only useful if it’s relevant to your business, and is clean. Additionally, you need to know the problem that you’re trying to solve.
There has been much focus on technology itself, yet as Bali Padda, former COO of LEGO once noted:
“Deploying the latest digital connectivity does not guarantee you have a modern, agile and high performing business, in the same way that owning a superbly engineered car won’t guarantee that you will be a great driver.”
In this regard, it’s important to note that while the digital revolution is real, and that technological breakthroughs do bring about considerable organisational and social benefits, this can only happen if human systems are already working well. The technology is just the car, you are the driver.
As Sanders and Wood noted in their article ‘The Secret to AI is People’:
“Our key takeaway is counterintuitive. Competing in the age of AI is not about being technology-driven perse—it’s a question of new organisational structures that use technology to bring out the best in people. The secret to making this work, we learned, is the business model itself, where machines and humans are integrated to complement each other. Machines do repetitive and automated tasks and will always be more precise and faster. However, those uniquely human skills of creativity, care, intuition, adaptability, and innovation are increasingly imperative to success.”
Key to successful automation is to be clear about:
■ what you are automating
■ why you are automating
■ how this contributes to your organisation’s value chain
Implicit in these considerations is the need to understand your business’ value and cost drivers, and to understand how these two drivers interplay with each other.
Our commercial imperatives in aged services involve reducing costs, and increasing efficiency and productivity. However, automating organisational processes without fully understanding the potential impacts on how our organisations deliver care, can lead to unintended counter-productive consequences.
In a nutshell, automating a bad organisational system is essentially doing wrong things more quickly.
Being in the business of caring for older persons, our digital tools and automated processes need to be aligned to existing human systems and consumer needs.
However, if you failed to deliver, gathering data and information is not enough.
Merlin Kong, Head of Innovation and Industry Development, Aged & Community Care Providers Association www.innovageing.org.au


The Federal Government’s Home Care Workforce Support Program’s aim is to attract Personal Care Workers, Enrolled Nurses and Allied Health Assistants to the home care sector of aged care, and to grow the workforce by 13,000 people over the next two years.
The Home Care Careers brand has been developed by the Consortium responsible for delivering the Program in Victoria and Tasmania, consisting of ACCPA, Human Services Skills Organisation (HSSO) and PowerHouse Hub (PHH). Through a united identity, approach and channel, the Consortium have already begun rolling a strategic plan to grow the home care workforce in each respective state.
The Home Care Careers web portal has been carefully developed by PHH to connect potential aged care workers with home care providers in a simple yet effective manner. Specifically, home care providers will enjoy the value proposition of a streamlined recruitment process, which utilises artificial intelligence to match candidates to the right jobs.
Candidates looking for part-time, full-time or casual work in the home care sector begin by registering on the Home Care Careers website.
While creating an account, candidates will be prompted to upload their resume and other supporting documents such as qualifications and compliance documentation to a personalised digital Workforce Wallet.
Through the analysis of each candidate’s preferred location and availability, the system can flag potential job matches. Specialist Talent Acquisition Consultants are then able to reach out to candidates to finalise the pre-screening process and connect the candidates directly with providers.
This pre-screening activity is a vital time saver for providers as candidates that are presented for employment opportunities are already considered to be a ‘right fit’ for the roles.
The Home Care Careers portal is being supported by a mass marketing campaign to attract job seekers to a career in home care, as a personal care worker, enrolled nurse or allied health assistant..
The campaign theme, devised by creative agency Cocogun, working with Impetus Media, is targeted to individuals who are best suited to work in these roles - “If care is in your DNA, consider a career in home care’.
One of the first mass candidate attraction campaigns involved a series of regional and metropolitan radio advertisements that aired in Victoria and Tasmania. These are broad reaching strategies aimed at sparking the interest of a range of potential candidates from career starters to career extenders.
The Home Care Careers team have also invested in cinema, out-of-home (transit), billboards, YouTube, search, broadcaster video on demand and online radio to maximise the reach of the campaign.
To provide an authentic touch to these advertising channels, real home care workers were engaged in the filming and
photography process to share their experience and stories. Since launching the marketing assets, the Home Care Careers website has seen a significant increase in traffic.
The Home Care Careers social media and digital marketing plan was also launched in October 2022, with accounts created for platforms such as Facebook and LinkedIn, featuring a series of blog posts written by job providers with the aim of attracting career leavers and career starters to the sector.
Through pairing these marketing efforts alongside the technically robust Home Care Careers portal, the Consortium aim to generate interest within and around the sector, and significantly grow candidate usage of the portal.
The Home Care Careers portal now offers home care providers operating in Victoria and Tasmania a new, streamlined channel and method for recruiting home care workers who fit the job description and requirements.
Sign up as a provider for the Home Care Careers portal today for free, and let the technology developed for you, work for you in recruitment and attraction of home care workers.

Omeed Shahriari, Marketing CoordinatorHome Care Workforce Support Program, Aged & Community Care Providers Association www.homecarecareers.com.au
ACCPA, HSSO and PHH are delivering the Federal Government’s Home Care Workforce Support Program in VIC/TAS. For more information about how to access new recruits in your state or territory, visit www.health.gov.au/initiatives-and-programs/homecare-workforce-support-program
Australia needs 100,000 more care workers by 2028, significantly more than the existing population of Coffs Harbour.
This confronting figure was the key finding from the Australian Government’s Care Workforce Labour Market Study conducted by the National Skills Commission, which revealed worse-than-expected labour shortfalls for the care sector.
While it might not come as a surprise, the figure does highlight the urgency of shifting our trajectory.
The more positive side to the report is the Government’s overt recognition of the industry’s plight and its commitment to ‘working to improve attraction, retention and the sustainability of the care workforce to deliver reform the sector so desperately needs’.
Australia’s policymakers have already committed to changing the sector’s outlook by establishing the nationwide Home
Care Workforce Support Program (HCWSP) to strengthen the personal care workforce.
SSI is proud to deliver the program in NSW and the ACT, and we are focused on placing 4,400 new home care workers into work and training in the next two years.
Since the program came to life in April, SSI has spoken with dozens of care providers and industry experts to learn about challenges and opportunities they’ve identified in finding and retaining qualified talent.
We have turned this wealth of information into insights to shape our program and better support the sector in its search for workers.
To encourage more people to build meaningful careers in home care, perceptions of the industry must change. We need to lead a discussion, bust myths and change views about home care through real, human storytelling.
We also need to differentiate at-home aged care from other care professions by highlighting it as a meaningful, unique and flexible long-term career pathway.
SSI started this journey by launching a multichannel marketing campaign, ‘Make a difference with every door you open’, that celebrates the life changing work home care offers.
This campaign will continue to be featured across social media, online and digital platforms over the coming months. Tackling misconceptions and negative perceptions of aged care with authenticity will benefit the industry by ultimately encouraging more people to consider entering the sector.

The program involves three stages for the participant: screening, assessment and onboarding. During each of these stages, we give participants the information they need to make an informed choice about their career. We then connect them with relevant training or work opportunities depending on their circumstance.
We also support our participants with police checks, working with children checks and first aid certificate training, among other essential qualifications. Once job-ready, we provide them with information on home care providers and help them with interview preparation.
This means by the time we connect a candidate with a potential employer, they will already be vetted and prepared. As a result, our partners can confidently hire the candidate quicker and more efficiently.
The Home Care Workforce Support Program is committed to supporting our participants beyond the recruitment process to ensure the transition into the workplace goes smoothly and is built to last.
We do this by offering regular check-ins, mentoring programs, continuous learning opportunities and peer groups to participants even after they begin work.
Another key objective for SSI is to design talent retention plans, which means we will help our partners build processes and strategies to keep their workers longer.
Our goal is to support our industry partners to build capacity for the sector for the long-term – not just to help tackle the skills shortage of today, but help the industry come together to change the direction Australia is headed when caring for our seniors.
This shift will be a victory for the community and all involved parties, especially our senior Australians who need quality support in their own homes.
Iggy Pintado, Head of the SSI Home Care Workforce Support Program www.ssi.org.au/homecare
SSI is delivering the Federal Government’s Home Care Workforce Support Program in NSW/ACT. For more information about how to access new recruits in your state or territory, visit www.health.gov.au/initiatives-and-programs/ home-care-workforce-support-program

For over 27 years Tender Loving Cuisine has been serving the community with care, compassion and respect. Australian Made and Owned, our health accredited, home delivered meals cater for dietary requirements with all meals developed and supported by independent review.

Our extensive menu also includes selections that are Dairy Free, Low Salt, Gluten Free, Heart and Diabetes Friendly. Our purpose is to assist clients to maintain their dignity and independence.
Assured nutrition, great taste, strict dietary controls and dedicated customer service is at the heart of what we do. With a trusted reputation and Industry Recognition, Tender Loving Cuisine sets the standard in quality and reliability. We proudly provide meals in Aged Care Packages, NDIS, CHSP and the general community in areas of QLD, NSW, ACT and VIC. Contact us for brochures or futher information, we’re here to help!

Recent reports have stated that Australia’s agedcare system is in crisis, predicting a shortfall of 200,000 jobs by the year 2050.

Apprenticeship Careers Australia is committed to finding solutions to this forecasted problem with programs such as the ‘Home Care Workforce Support Program’, currently being delivered in South Australia and Northern Territory. This initiative is part of the Federal Government’s commitment to increasing the healthcare sector’s workforce and supporting Australia’s elderly community that wishes to live independently in their homes for longer.
This is off the back of a recent successful program, ‘More Jobs More Care’, which delivered 300 trainee placements and over 1,700 people employed in the disability support industry, along with some welcome findings.
Luke Radford, National General Manager of Apprenticeship Careers Australia said, “Provider feedback indicated that employing trainees had reduced staff overtime, which had a significant positive impact on their bottom line, and allowed them to focus on other priorities in delivering quality care for their clients.”
In an industry bouyed by casual workers, it is a little-known fact that trainees can be employed in order to fill the gap. Brett Clarke, NSW/ACT State Manager encourages businesses to
consider alternatives. “We strongly believe the industry should look to the uptake of a more structured pathway into the sector for new starters and this should be via an accredited traineeship rather than a casual workforce,” said Brett.
Apprenticeship Careers Australia has expertise in running small localised recruitment campaigns as well as larger statewide projects, sourcing talented people who have an initial interest in the care sector, preparing them for job readiness, and supporting them via the traineeship model over the longer term.
“We are very confident this will reduce the turnover in the industry which relies heavily on a casual workforce, thus bringing career pathways and mentoring support to the new trainee entrants, also providing a more qualified and professional care workforce with increased standards of service to the providers and their clients within the care sector,” said Brett.
Becoming an Aged and Community Care Providers Association (ACCPA) Partner is another advantage.
“The connection with ACCPA allows us to be in a unique and privileged position to deliver practical proven workforce solutions for the sector, it also helps us understand the challenges from those on the frontline of healthcare,” said Christopher Fox, National Recruitment Manager at Apprenticeship Careers Australia.
future-proofing their employability in the healthcare sector
The successful rollout of ‘More Jobs More Care’ program also revealed that the majority of candidates applying for traineeships were mature-aged people looking for a career change, wanting to upskill and gain qualifications in a new field, rather than the traditional youth trainee applicant.

Luke Radford adds, “Applicants are searching to future-proof their employability in an industry where there is high demand for skilled people.
“Our programs create an incredible opportunity for Australian providers and the wider community, young and old, by providing a mutually beneficial solution or at the very least offsetting the impact of the care crisis.



“We as an organisation are guided by our values – care, courage, collaboration, and inclusiveness – and are committed to finding solutions to support our community into the future.”

Peta Bormann, Communications Manager, My Business www.apprenticeshipcareers.com.au
Apprenticeship Careers Australia is delivering the Federal Government’s ‘Home Care Workforce Support Program’ in SA/NT. For more information about how to access new recruits in your state or territory, visit www.health.gov.au/initiatives-and-programs/ home-care-workforce-support-program

Development of the new, unified Support at Home Program is underway, with initial proposals outlined in an overview released by the Department of Health (and Aged Care) in January 2022 and further detail in a discussion paper released in October 2022. Support at Home will replace the Commonwealth Home Support Programme, Home Care Packages, and the Short Term Restorative Care program.

The incoming Minister for Aged Care has deferred the start date of the program by one year, to 1 July 2024. Minister Wells said that this would enable further consultation and ensure that reforms will “bring genuine improvements for older Australians in the long and short-term”.
Many of the proposed changes have merit. A new Integrated Assessment process will provide a single, simplified pathway for access to subsidised aged care services, and the inclusion of restorative care as a dedicated category within the Classification Framework has the potential to open up access to these valuable services to a greater number of older people. The development of a comprehensive Service List for the program will provide much needed clarity and consistency around service offerings, especially in the case of access to goods, equipment and assistive technologies.
Nonetheless, questions remain about how the proposed reforms will affect consumer choice and control, provider accountability, and the sustainability of publicly subsidised in-home aged care.
The new, fee-for-service model will give older Australians the freedom to choose from a range of approved providers. This can be expected to strengthen consumer choice and control. However, the potential delivery of services by multiple providers may make it more difficult for clients to hold individual providers to account.
There are also broader issues of accountability between the roles of assessors who determine the services to be provided,
care managers who work with older Australians who have complex needs, and the providers of the services. If services don’t deliver good outcomes, who is responsible?
Older Australians inevitably have changing needs and the design of the new program will need clear and efficient mechanisms for modifying Individualised Support Plans in a timely manner. Right now, it is unclear who can seek or approve changes. It is similarly unclear who in this arrangement will advocate on behalf of older Australians, particularly where assessors have not provided for care management in the plans.
Furthermore, the development of a comprehensive service catalogue and a corresponding ‘efficient’ price list may create rigidities which constrain consumer choice and competition. This is because fixed prices, while potentially improving transparency, will limit the ability of providers to compete on price and threaten the viability of more costly service provision, such as in regional, rural and remote areas.
Currently about 90 per cent of in-home program costs are borne by taxpayers. This is not sustainable.
Getting the design of the Support at Home program right in the first instance will be crucial for the independence and wellbeing of senior Australians, for clear accountability between the various roles in the system and for the long-term sustainability of aged care.
The UTS Ageing Research Collaborative has developed a Support at Home report that provides detailed commentary on the design of the planned changes, raises key concerns, highlights strengths and shortcomings, and proposes a series of options for how the cost of in-home care could be more equitably shared between taxpayers and those clients who have the financial capacity to make a reasonable contribution.
Dr Rachael Lewis, Lecturer, UNSW Business School and Founding Member, UTS Ageing Research Collaborative www.uts.edu.au/uarc/news/report-support-home





We know early diagnosis of dementia can lead to better health outcomes, and now two simple physical measures may enable health professionals to identify older adults at highest risk of developing dementia in the future.
New research from Monash University has found poor gait (walking) speed and grip strength could be early indicators of dementia, before noticeable symptoms emerge.
Slow walking speed combined with weak hand grip was a stronger predictor of cognitive decline and dementia in older adults than either measure alone.
Early identification of high risk individuals enables health care professionals to implement intervention strategies to reduce risk, possibly slowing disease progression and improving patient outcomes.
Published in the September 2022 journal Alzheimer’s & Dementia: Diagnosis, Assessment & Disease Monitoring, the study analysed data from more than 18,000 participants enrolled in ASPREE, a long-term bi-national clinical aspirin trial in initially healthy older adults, mostly over the age of 70. (For more information about ASPREE, visit www.aspree.org/aus/)
Participants’ grip strength and gait speed was measured upon entry to ASPREE and repeated during an average of 4.7 years. Gait speed was timed walking at normal pace over a distance of three metres, while grip strength was assessed using a hand-held device to measure force. These physical benchmarks were measured against cognition assessments.
Researchers found a combined poor gait speed and grip strength was linked to a 79 per cent increased risk of dementia and a 43 per cent increased risk of cognitive decline. Over time, the risk for dementia or cognitive decline was highest when gait and grip declined simultaneously over almost five years, with an 89 per cent increased risk of dementia and 55 per cent increased risk of cognitive decline. This is the first time these two physical measures have been combined together to assess the link with cognitive decline and dementia.
Given grip strength and gait speed are low cost and easy to administer assessment tools, the study could have significant implications for detection and treatment as the number of people living with dementia is expected to grow from 57.4 million in 2019, to 152.8 million by 2050.

During the course of the ASPREE trial, 2,773 participants in this analysis developed cognitive decline and 558 dementia.
The grip instrument used in the ASPREE study could become part of a low-cost method for identifying early signs of dementia.
Lead author Dr Suzanne Orchard, a Senior Research Fellow with Monash University’s School of Public Health and Preventive Medicine, is the Australian director of ASPREE-XT, the observational follow-up study.
Dr Orchard cautions that having poor gait and grip does not guarantee someone will develop cognitive decline or dementia. However, she says identifying this important link between age-related cognitive and physical decline could benefit those who are at risk.
“We hope that understanding this association will enhance early detection and prevention strategies,” she said.
“While there is no cure for dementia, older adults identified as being at risk of cognitive decline and dementia may benefit from physical, social and mentally stimulating activities, having a healthy diet, good control of blood pressure and diabetes, not smoking and reducing other risk factors for dementia.”
ASPREE was funded by the National Institutes of Health (NIH in the USA) and NHMRC, Monash University and the Victorian Cancer Agency.
ASPREE communications team, School of Public Health & Preventative Medicine, Monash University www.monash.edu/medicine/sphpm
Slow gait and weak hand grip combined warrants investigation
For a long time, the Aged and Disability Care sector in Australia has been looking for their software providers to offer a fully integrated solution to drive efficiencies by scheduling services, maintain compliance and seamlessly manage payroll, billing, account management and general ledger.
Care Systems ensures
■ Rostering and scheduling is managed efficiently.

■ Overstated KMS (both between and during service delivery) are eliminated.
■ Staff receive the information they need to be effective in their role of delivering quality care.
■ Employees are paid in line with the relevant EA or Award. On time – every time.
■ Clients receive accurate and compliant statements and invoices with no manual data transfer or need for 3rd party integrations.
■ Your organisation maintains compliance while delivering quality services to your clients.
■ Government reporting is generated without the need to import/export data.
Care Systems has listened to what its clients and the market are asking for, and are proud to deliver its suite of fully integrated and cloud-hosted applications that will create efficiency and support compliance for any organisation in the Aged and Disability Care sector.

Ensuring your compliance is maintained From front-end home and residential client management and service rostering with the support worker mobility app, to resident billing, ACFI calculation, back-end payroll, billing, accounts and government reporting
Using the latest Care Systems cloud technology, payroll and client billing is simple and streamlined. Care Systems’ HomeCare and HomeCare Mobile modules seamlessly integrate to manage your rostering, filling empty shifts quickly and easily, while managing your KMS, worker skills and client preferences.
Once services are completed, real time mobile time and attendance data is matched to rostered shifts and services, enabling swift approval and processing of Payroll.


Want to maximise revenue and ensure effective and compliant Client and Resident Billing? Care Systems supports providers to maximise their funding entitlements and ensure Clients and Residents are billed correctly. We can manage your Medicare payment statement reconciliation and analysis to ensure you don’t miss out on funding entitlements, payments and supplements.
As clients are billed directly from the system, end of month reconciliation and reporting occurs in parallel.
Have peace of mind knowing your residents are billed correctly, and your staff are paid accurately and on time.
Indoor air quality has always been important, however with the continued airborne spread of SARS-CoV-2, it is more important than ever for aged care facilities to take action for the safety of their staff and residents by doing all they can to minimise the spread of airbourne viruses.

Used in hospitals and clinics throughout Australia, InovaAir® air purifiers are an extremely effective tool to improve indoor air hygiene.
Each system utilises a high-efficiency pre-filter and medicalgrade HEPA filter to capture airborne aerosols, viruses, bacteria, pollens, allergens and mould spores.
Unlike some of the plastic alternatives, InovaAir uses powder-coated aluminium construction making them well suited to commercial environments where disinfection is regularly required.
InovaAir® systems also include long-life filters providing up to 3 years between changes*
Proudly Australian owned and manufactured on the Central Coast of NSW for 20 years.
High capacity, cylindrical H13 certified medical-grade HEPA filter with 6.4m2 surface area and metal casing.
Plastic-free, chemical-free, aluminium powder-coated construction allows for easy wipe-down and disinfection of external surfaces with any ethanol-based alcohol cleaning agent.
Directional High-Flow™ air diffuser for quiet operation and superior airflow.


Australian made, ensuring quick and reliable support and filter replenishment.
Portable. Easily moved from room to room on wheels. Wall mounted versions also available.
100% Airtight filter seals.
www.inovaairpurifiers.com.au/agedcare
At the International Dementia Conference 2022, I and my colleagues Professor Colm Cunningham and Dr Madeleine Healey launched BPSD Textbook: Addressing behaviours and psychological symptoms of dementia

We believe the release of this textbook on managing behaviours and psychological symptoms of dementia (BPSD) is a milestone in establishing non-pharmacological treatment, rather than medication and restraint, as best practice.
BPSD Textbook is also a personal milestone, after a profound change in my professional journey that began seven years ago, 12 years after I became a geriatric psychiatrist
On a sabbatical from my job as head of aged psychiatry at Alfred Health, I joined a HammondCare project that was developing severe behavioural response teams (SBRT).
I’d been aware, of course, that behavioural, psychological and environmental interventions should be the first line of treatment for behaviours and only if they failed should we use medications.
Yet most of the people in my public hospital wards were medicated. Until that point in 2015, I had assumed we used medications because non-pharmacological treatments usually didn’t work.
But my training as a geriatric psychiatrist hadn’t equipped me even to do the assessments necessary to establish individualised behaviour-modifying treatments, let alone implement them as HammondCare teams were doing.
After six months working with the SBRT project and seeing the remarkable results being achieved, especially by comparison with my ward experiences, I resigned my public hospital position; I was a convert to the cause of non-pharmacological treatment of behaviour change in dementia.
Our research since only confirms that the evidence to support using any medication in BPSD is very limited and even in those cases where there is any convincing evidence, the effects are small and the side-effects are significant.
And yet, we estimate more than 70 per cent of people living with dementia in residential care are prescribed at least one psychotropic medication, while some 30 per cent receive antipsychotics.
Very often, the behaviours being medicated are not symptoms of the dementia itself; as Colm writes in BPSD Textbook they are “on too many occasions, a reasonable response to unmet needs and circumstances a person with dementia will face”.
Madeleine, Colm and I have compiled and edited BPSD Textbook as a manual for all health and aged care workers, including family carers at home.
Up to 90 per cent of people living with dementia will experience forms of BPSD and, in aged care particularly, we seek to reshape the approach towards understanding and seeing the person, rather than their behaviours.
BPSD Textbook brings together our learnings, from HammondCare’s 25 years’ experience, and more recently from SBRT and Dementia Behaviour Management Advisory Service, to provide a solid grounding, not only in dementia and its biological underpinnings, but also in identifying and assessing the factors contributing to behaviours.
Because this is about training, as much as anything else. It is right and proper, as the Royal Commission into Aged Care recommends, that there should be more nurses in aged care homes, but those nurses need to know something about managing dementia.
How to manage behaviours without resort to medication is a big gap in the skill sets of most people involved, doctors and nurses as well as aged carers.
We need to make dementia and BPSD a more prominent component of aged care training but also of the medical and nursing curricula.
Without comprehensive improvement in training across aged care, nursing, medical and allied health services, I fear all the other Royal Commission recommendations in relation to dementia care might not be implementable.
Associate Professor Stephen Macfarlane, Head of Clinical Services for Dementia Support Australia (led by HammondCare) www.hammond.com.au/shop/ dementia-and-aged-care/the-bpsd-textbook
How a personal journey of discovery led to an essential manual for carersThe BPSD Textbook is packed with HammondCare’s learnings over 25 years.
There’s an expression you may have heard before, ‘you can’t teach an old dog new tricks’. It’s a catchy turn of phrase, and an idea which is often applied to older people too – a stereotype that with age comes stagnation. However, as is the case with most stereotypes, this expectation has been proven false time and time again.
At the National Ageing Research Institute, we see older people learning, growing and innovating every day. In particular, through the use of our ENJOY Seniors Exercise Parks.
The World Health Organisation (WHO) and Australian Department of Health and Aged Care recommend people aged 65 and older do about 30 minutes of exercise most days of the week. Unfortunately, only 25 per cent of older people in Australia currently meet these guidelines – it’s clear we need to rethink how outdoor spaces can best be designed so they offer opportunities for older people to get moving, in a safe environment.
The ENJOY (Exercise interveNtion outdoor proJect in the cOmmunitY) project has seen the development of 14 Seniors Exercise Park across Victoria, with more planned for locations interstate.

These spaces are designed to specifically cater to the wants and needs of older people, featuring a range of outdoor exercise equipment to help improve balance, strength, functional movement, joint range of motion and mobility. Importantly, these exercise parks are spaces for fostering both physical and mental wellbeing in older people. They are spaces for socialising, offering a new avenue for connection and purpose to someone who may otherwise be struggling.
Having outdoor public spaces, including parks, leisure centres and outdoor exercise equipment that is designed to be inclusive of all ages and abilities, is vital to allowing older people to age well.
Outdoor exercise has been shown to improve mood and self-esteem in older adults, and can also reduce feelings of loneliness and social isolation. Having local governments, and communities as a whole, get behind these projects and show their commitment to the health and wellbeing of older people is essential.
At NARI, we are proud to see our research brought to life
with these exercise parks becoming more widely available to older people in our communities, and would like to see access to such an important resource in every neighbourhood. Creating outdoor spaces that are inclusive and accessible provide vital opportunities for older adults to engage in physical activity and social interaction, both of which are central to healthy ageing.
Yet another benefit of the ENJOY project is the fostering of intergenerational connections throughout the community. By establishing Seniors Exercise Parks in pre-existing community spaces, older people have further opportunity to meet and get to know people of all ages. Research has proven such intergeneration relationships are hugely valuable to ageing well.
Participants in NARI’s ENJOY Seniors Exercise Park physical activity program have shown significant improvements in physical strength and functional mobility, which were sustained long term.
Their physical activity level also increased from sedentary to being sufficiently active to gain health benefits. They also rated quality of life, wellbeing, fear of falls, falls risk, depressive symptoms and loneliness as significantly improved.
So, in fact, new tricks can be learned at any age – especially when the right tools and spaces are provided to those willing to give it a try.
Professor Pazit Levinger, Principal Researcher and Project Lead of the ENJOY project, National Ageing Research Institute www.nari.net.au
In October this year, Lutheran Services’ residents from across Queensland performed in an intergenerational dance show at the Queensland Performing Arts Centre’s (QPAC) Cremorne Theatre – demonstrating the value of bringing the young and old together.
The moving performance ‘If Only I Could…’ was met with applause and cheers from the audience, who were wowed and amazed by the talents of the dancers.
Six residents of Lutheran Services’ Tabeel Aged Care, along with professional dancers from across Queensland, recently took to the stage in a performance that showed the power of movement and connectivity, and that age is just a number.

The concept for ‘If Only I Could…’ began five years ago with Director Angela Chaplin running a series of dance workshops with Lutheran Services aged care residents.
“This project came from my belief that everyone in our diverse community – no matter their age – should have the opportunity to explore their creativity,” said Angela.
Lutheran Services Creative Programs Advisor Clare Apelt said that ‘If Only I Could…’ was created to breathe life and colour into residents’ lives, with opportunities to move and connect with others.
“We know there is a direct positive correlation between music and movement, and older peoples’ health and wellbeing – both mental and physical – so creating an opportunity for them to be involved in a project of this kind was truly rewarding,” said Clare.
“It was great to witness the growth in our residents’ lives and the happiness being involved this dance performance brought them.”
Rehearsals for ‘If Only I Could…’ took place over several months and offered residents a sense of purpose and direction as they formed new friendships, re-discovered their confidence, and tested the abilities of their bodies and minds.
Preparation for the performance included dance workshops alongside some of Queensland’s foremost contemporary professional dancers.
One Lutheran Services’ Tabeel Aged Care resident who took part in the performance was 76-year-old Michael Bailey.
After breaking his knees and shoulder earlier this year, and being told he could never walk again, Michael defied the odds and showed that with the right attitude and spirit, anything is possible.
Director Angela Chaplin, whose works have toured across the country and internationally, said that directing this performance was a moving experience.
“Witnessing the relationship and trust created between the dance artists and our elder performers, while celebrating the big lives of our elder collaborators, was incredibly rewarding,” said Angela.
“This dance project showed that no matter our age or physical abilities, the stage belongs to all of us.”
Marking the third year of ‘If Only I Could…’, with performances previously run at the Judith Wright Arts Centre in 2018 and the Laidley Cultural Centre in 2021, the 2022 performance at QPAC boasted the biggest stage and audience to date.
Lutheran Services would like to thank its partners Premier Partner LLL Australia, Partner Cable Comm and Sponsors Bidfood Australia and Productivity for their generous support of the performance, and QPAC, the co-presenter of ‘If Only I Could…’ for their ongoing support.
Lutheran Services www.lutheranservices.org.au



Policies provide guidance, consistency, accountability, efficiency, and clarity on how your organisation (residential care or home care) operates. This enables your team to understand your organisation’s philosophy and guiding best practice principles. Policies are not just a compliance requirement. They are a vital component of good governance and set parameters for all elements of your organisation. Without adequate and well-developed policies there are no rules, and unfortunately, without defined rules, people create their own. Good policies link an organisation’s vision, values and day-to-day operations and identify key activities and guide decision-makers on how to handle issues as they arise. The importance of policies cannot be overlooked. Without them, your organisation is exposed to risk.
Anchor Excellence’s suite of evidence-based best practice policies will; support your compliance, improve internal processes, help you navigate incidents & issues that arise, increase understanding of expected behaviours and performance standards in your team, provide rules for the decision-making process across your organisation.




Processes have a vital role to play in the efficient and effective functioning of aged care organisations. In addition to driving efficiency and compliance, processes are important because they provide a step-by-step best practice guide that describes how things are done. Processes need to be evidence-based, best practice, well-designed, communicated effectively and document controlled if you want to set your teams on the right path to success. With clear processes in place, your team will understand their responsibilities, roles and delegation, which in turn will lead to an increase in productivity, improved workflow management and improved consumer health and wellbeing outcomes.
Anchor Excellence’s suite of processes, tools, frameworks and manuals can to reduce risk, reduce human error and improve efficiencies, collaboration and consumer health outcomes, as well as ensure effective communication across multi-disciplinary teams.
Practice is a combination of ensuring you embed your policies and processes as a part of your culture and Model Of Care. Your team need to fully understand their roles and responsibilities and what best practice looks like. Education plays a significant role in embedding best practice in aged care. The capabilities of your Management, Care Teams and General Service Teams have a direct correlation to safe and quality care and compliance with the Aged Care Quality Standards. Skilled and qualified aged care professionals are the key ingredient to minimising risk to older Australians and improving their health and wellbeing outcomes.
Anchor Academy follows an evidence-based, best-practice framework that is aligned with the Aged Care Quality Standards. All education, including (but not limited to) key personnel, assessment visit readiness, clinical management and governance, new graduate, restrictive practice, SIRS, and reform agenda updates, are designed to increase knowledge, improve performance and capability and assist aged care providers to meet and exceed their compliance obligations.
If you are looking at implementing a connected medication management system, now is the time to apply maximise grant benefits of up to $22,000 per site.


Although we are wholly focused on medication management, BESTMED understands the importance of a connected medication management system and is dedicated to growing our integration partnerships to help streamline your systems allowing you to focus on care.
Are you eNRMC ready?
Scan the QR code for information about the eNRMC adoption grant opportunity funding currently available, or to book a demonstration contact:
An estimated 85 per cent of residents in aged care homes in Australia have a hearing impairment – however, the number who have hearing aids is substantially less. With that in mind, Hearing Australia, provider of expert hearing care and world leading research for 75 years, is calling on aged care facilities to prioritise hearing health for their residents.
“Those living in residential aged care homes are more likely to have hearing loss compared to those living in the general community. Increasing longevity and the older demographic of aged care residents means a growing incidence of hearing loss among this cohort,” explains Emma Scanlan, Principal Audiologist for Adults with Hearing Australia.
“Unfortunately, under-detection of hearing loss and underuse of hearing aids is prevalent in aged care homes, which can be a major barrier to optimal hearing and communication for residents.
“In addition, residents often have other co-morbidities, which means prioritising hearing support is even greater. For example, if someone with cognitive impairment also has hearing loss, they need more hearing help, because it impacts their ability to communicate.”
To help address the issue, Emma says it’s important for aged care homes to put in place hearing health programs.
“We recommend a program that starts from a resident’s intake, ensuring they have a hearing test conducted by an audiologist at the outset, and residents should then have an annual examination to keep on top of any deterioration in hearing,” she said.
“It’s vital to have a well-supported program whereby hearing specialists come in to check residents and follow the appropriate path according to what funding is available.
“The earlier you intervene, the better the outcome.”
It’s equally important for residents and family members to prioritise health programs when looking for an aged care home, when looking for a provider of quality care.
Things to review in your health and wellbeing program include:
■ Is there regular contact with a good hearing provider?
■ Is there a hearing check at intake?
■ What percentage of residents have and actually use hearing aids?
■ Is there any special hearing equipment for residents to use and do the staff have an ongoing education program about hearing loss support?
The consequences of hearing impairment for aged care residents include isolation, loneliness, depression, missing out on social activities, and the inability to communicate needs.
“Hearing loss reduces your ability to communicate in all situations and reduces quality of life,” says Emma. “It can complicate both the provision of care and support of quality of life for residents. In addition, if you have hearing loss, there’s a greater chance of developing dementia.”
Hearing Australia provides a full range of services in aged care facilities as well as in its hearing centres. That includes hearing assessments, hearing aid fittings and rehabilitation appointments. And its services don’t end with the residents. Hearing Australia also offers free staff training that focuses on caring for residents’ hearing needs in aged care, as well as providing helpful information about enhancing their environments, such as reducing noise, furniture placement to make communication easier, and troubleshooting for devices like hearing aids.
Key tips for nursing and support staff caring for hearing impaired aged care residents include:
■ Clear communication. Reducing background noise is crucial. When you reduce noise and then speak with someone face-to-face, most people have a better chance of being able to communicate.
■ Hearing checks. Ensure all residents have their hearing checked when they move into an aged care home and, for those with a hearing impairment, support them to get help.
■ Get familiar with hearing aids. A lot of carers are nervous about touching hearing aids because they can be a high cost item. But if you receive some training, you’ll know how to help residents with maintaining their devices. It’s important for staff to have basic troubleshooting skills, which might be as simple as changing batteries.

Hearing Australia provides subsidised hearing services to eligible aged care residents including pensioners and veterans. Conditions apply under the Australian Government Hearing Services Program (HSP). The NDIS and My Aged Care also provide some hearing services funding for those who meet funding criteria.
Hearing Australia www.hearing.com.au
Food Solutions is a leading Australian provider of aged care Dietitians and Speech Pathologists.
Up to 60% of aged care residents are likely to be at risk of or experience malnutrition. Our Dietitians will combine clinical and food service expertise to optimise nutrition and good health for these residents.
Approximately 70% of residents in aged care experience dysphagia. Our Speech Pathologists specialise in the assessment and management of swallowing difficulties and can provide support and education to carers and aged care staff.
Our foodservice programs support the full menu process from design through to review. Dietitian and Speech Pathology intervention tailored to meet your needs.
It is essential to get modified diet and fluids right every time! Our training and auditing programs will ensure your facility is compliant.
Our reviews offer a holistic and independent assessment of the mealtime and dining experience with support programs for improvement.
Our team optimise resident’s nutrition, hydration and safety as well as assisting food services to promote health, wellbeing and quality of life. We’d make a
We are passionate about education. Our online and face-to-face education programs cover a range of nutrition and dysphagia topics suitable for clinical, care and food service staff.
Access quality care, close to home. For your convenience, Food Solutions offers Speech Pathology and Dietetics directly into your facility via Telehealth.
Mealtimes and mid-meal times can be the highlight of every day for those living in residential aged care homes.
The mealtime experience can influence both the amount of food eaten and the level of nutrition achieved. It can also add joy and improve the quality of life of your residents, if care is taken to ensure a positive environment.
With up to 60 per cent of aged care residents at risk or suffering from malnutrition, it is crucial that we get the food and nutrition right.
By undertaking a thorough review of your meal and mid-meal service delivery, you can find areas of improvement in both meal preparation and the mealtime experience.
■ Is the dining room environment peaceful, happy and welcoming?
■ Are your residents sitting comfortably at the table, with their friends, and able to enjoy the social atmosphere?
■ Can your residents see their meals, with coloured placemats on the tables that contrast with the colour of the plates?
■ Is the meal appetising and does it stimulate the senses –sight, smell, taste, feel?
■ Are the meals pleasing to look at and filled with a variety of colour?
■ Are the meals served at the correct temperature?
■ Does the aroma of the meals make you want to continue eating?
■ Does the menu provide sufficient variety?
■ Have your residents been included in planning the meal choices so that they get to enjoy their favourite foods?
■ Are your residents getting enough to eat and drink?
■ Are the staff available and willing to help the residents when they are unable to help themselves, and prompt and encourage them to consume sufficient quantities?
■ Do the staff engage the residents in conversation at mealtimes and make them feel special, regardless of how fast or slow they are able to eat?
■ Given the freedom of choice, would your residents visit your restaurant again?
Choking is the second most common cause of preventable death in residential aged care in Australia, and the leading cause of premature death in people under the age of 65 in residential care. By ensuring that your residents are provided
with the correct textures at mealtimes, you can help them consume food easily and safely.
■ Support your residents to be positioned correctly (90 degrees upright) for oral intake, and ensure that they have all necessary equipment for the meal, including dentures and glasses.
■ Reduce unnecessary distractions in mealtime environments, so that residents can concentrate on their meals.
■ Ensure that the resident is receiving the correct diet texture that has been prescribed for them. Food must meet International Dysphagia Diet Standardisation Initiative (IDDSI) requirements, which specify how soft the food needs to be and how big the food particles are. If a resident is given food that is harder or larger than what they have been prescribed, then they are at an increased risk of choking on that food.
■ Provide assistance or supervision to residents with their meals if this has been recommended for them. This means that any difficulties can swiftly be addressed if they arise.
Oral disease can cause pain, result in poor nutrition or potentially place a resident at an increased risk of aspiration pneumonia or systemic conditions such as cerebrovascular disease. Residents need to be able to eat and talk comfortably, stay free of oral pain and maintain self-esteem in their oral hygiene and care. Be sure to support residents with their oral cares when they are unable to do so themselves.
Dietitians and speech pathologists can work closely and collaboratively with your teams to ensure that residents are allowed to dine with dignity by ensuring that meals provided are in line with the IDDSI standards, strategies are suggested to improve the overall mealtime experience and mealtime safety and residents oral health is prioritised.
Seeking out advice from diet consultants such as Food Solutions can make a big difference to your residents and your ability to maintain compliance. Food Solutions specialises in aged care and can assist with all aspects of the dining experience and tailor a package to suit your needs.

Food Solutions
www.foodsolutions.com.au
How you can improve the mealtime experience for your residents
Effective cleaning and disinfection of surfaces and equipment is essential to any aged care infection prevention program.

Selection of the right products can prevent infections by removing harmful microorganisms (germs) helping to keep your residents, visitors and staff safe. Here are a few tips and reminders to help you make sure your infection prevention and control (IPC) program is best-practice.
Detergents help lift dirt and germs for easier removal from a surface but have no capacity to kill germs, whereas disinfectants kill germs rather than clean them away. Organic soil reduces the ability of disinfectants to kill, so surfaces need to be precleaned with a detergent before the use of a disinfectant.
High-touch surfaces and shared equipment (e.g. door handles, light switches, call bells, patient tables, chairs) pose a high risk of becoming contaminated with germs and being transferred to other people, potentially causing infection.
High-touch surfaces are touched most frequently by the resident, visitor or healthcare worker and should be cleaned at least daily and when visibly soiled.
Shared equipment can act as a vehicle for infectious agents to be transferred from person-to-person and should be cleaned in-between use.
Poor cleaning technique can re-contaminate a surface. The 5 Principles of Cleaning is a clinical resource that can be followed to improve cleaning technique. This is a methodical approach designed to minimise the risk of transmission of germs from one surface to another, which you can ask your staff to adopt in your aged care setting.

There are two main considerations when selecting a cleaning product: efficacy and contact time.
Products that remove 99 per cent of germs may seem impressive, but given there could be millions of germs on the surface this would still leave thousands of germs behind, which still poses a risk of causing infection.
This is where a higher number like 99.99 per cent in a disinfectant offers greater protection and efficacy. Some germs can be more difficult to kill so it’s also important to select a disinfectant that is effective against those that pose the greatest risk.
Contact time refers to the time that a disinfectant must remain in contact with surfaces to kill germs. If the instructions for use state a contact time of two minutes, the product must stay damp and in contact with the surface for a full two minutes to ensure that the germs are killed. Removal or drying off before this time risks ineffective disinfection.
Contact times in the product you select should be realistic and achievable. Long contact times may be difficult to achieve due to time limitations or evaporation before the disinfectant has a chance to kill the germs.
Ryan Clarke RN, CNE, Clinical Nurse Educator, GAMA Healthcare www.gamahealthcare.com.au
Hygiene has always been a key consideration in the aged care sector, but with the advent of COVID-19, the spotlight is even more focused on the eradication of germs, bacteria and viruses.
Healthcare workers and older people have been disproportionately impacted by the pandemic, and the need to protect aged care staff and residents has never been more important.
As a result, there has been a significant increase in the use of disinfectants and hand sanitisers, which has resulted in a corresponding rise in skin irritations caused by prolonged exposure to harsh chemicals.
In response, Ross Macdougald from BioInnovate decided to utilise his expertise to create a hand sanitiser that his wife could use without inflaming her eczema.
He knew that the ethanol and alcohol in standard hand sanitisers were the ingredients that were causing her skin irritation, so he researched how to create a plant-based sanitiser that would be effective, yet kind to her hands.
After experimenting with various compounds, he discovered that by adding chamomile and native lemon bush to the formula, he could reduce the active ingredient of benzalkonium chloride (BKC) to just 0.12% w/w, to create a highly effective hand sanitiser that kills 99.99% of germs and bacteria while still protecting the integrity of the skin.
“Anyone who has to apply hand sanitiser multiple times a day is well acquainted with how it can start to rip into your skin, causing redness, soreness, and even infection, plus a worsening of dermatitis and eczema,” says Ross.
He soon realised there were wider applications for his unique antimicrobial sanitiser, so he expanded the ViroCLEAR range to include a hospital grade disinfectant and a Sanitiser & Protectant Fogger.
Listed with the Australian Register of Therapeutic Goods, the VioCLEAR Hospital Grade Disinfectant is laboratory-proven to kill COVID-19, SARS, rhinovirus (the main culprit behind the common cold) within 90 seconds, candida albicans (which causes athlete’s foot, tinea, skin and nail infections) within 60 seconds, and 99.99% of germs and bacteria.
“In aged care settings, residents and staff are vulnerable to infection, so anything you can do to reduce the number of pathogens
they come into contact with is going to lead to better health outcomes,” says Ross.
“In addition, ViroCLEAR is non-flammable, non-toxic, safe for older people, children and pregnant women, and also safe for aquatic life,” he says.
The newest addition to the ViroCLEAR range is the Sanitiser & Protectant Fogger, which works much like a cockroach bomb. With the push of a button, the fogger dispenses a fine mist of anti-microbial sanitiser that gets into every crack and crevice to create a protective layer covering up to 40 square metres.
A game changer for aged care, healthcare, childcare and any indoor space that requires sanitisation, the ‘sanitisation in a can’ saves time, money and resources – essential considerations in healthcare settings.

“We believe there’s nothing else quite like this on the market,” says Ross. “The whole ViroCLEAR range circumnavigates the issue of high chemical load by leveraging nature, and best of all, it’s an all-Australian made and owned innovation.”
ViroCLEAR has just been announced as a finalist in the Best Retail Product Innovation category in the respected Finder Awards 2022. The ViroCLEAR suite of products is proudly distributed by Aussie Pharma Direct.
Daniel Seldon, Managing Director, Aussie Pharma Direct www.aussiepharmadirect.com.au
tailored specifically to your cooking

Request a Demo


A choice of cost effective tray sealing machiner y for DualPak trays is also available, from ergonomic and convenient benchtop sealers to inline automatic models. Contact your Confoil representative today for a demonstration of our tray sealing machiner y options.


Until recently the term ‘ageism’ was hardly known or used, even though the problem was recognised and given a name decades ago. Thankfully though, in just a few short years, ageism – stereotyping, discrimination and mistreatment based solely upon age – has leapt into public consciousness with force.
When it is directed against older people, ageism comes from the low value attached to older life, and negative attitudes and beliefs about what it means to be older. It can undermine our confidence, quality of life, job prospects, health, independence and control over life decisions. According to the World Health Organisation (WHO), it can even shorten our lives by several years.
In Australia and across the world, we now have campaigns to end ageism and ensure older people can access the same human rights protections as people at all other ages. Our own national coalition and grassroots campaign, EveryAGE Counts, has been recognised internationally as a leader in tackling ageism. Our ‘Take the Pledge to End Ageism’ has become a rallying cry for Australians to commit to making our society fairer and more inclusive for all ages.
One of the pernicious hallmarks of ageism is that all people over about the age of 60 are stereotyped as ‘old’, and the same as each other. This is despite huge diversity among this group of people. For a start, there can be up to 40 years’ age range among them. Then of course the differences in background, personal circumstances, identity and life experiences are also very deep and wide.
At EveryAGE Counts, we recently challenged the lumping together of all people at older ages into a single, homogenised group through polling we undertook for Ageism Awareness Day (held on 7 October). We surveyed and analysed responses from people over 50 in 10-year age cohorts. This enabled us to see how ageism is experienced and viewed by different older age sets.
A key finding was that seven in ten older Australians believe ageism against older people is a serious problem, but those in their 50s and 60s are significantly more likely to hold this view than those in their 80s and 90s.
How do we explain this startling finding, which to many of us is not intuitive? Surely, ageism is at its worst in experiences such as elder abuse in some families and in some care settings, patronising and demeaning interactions and high levels of social isolation, often experienced most seriously by those in the oldest age ranges?
Our polling did not give us the answer to these questions, but we can hypothesise one potential explanation. Given the relatively recent emergence of awareness of ageism,
it is possible that those in the younger range of older age now have a way of identifying, naming and resisting the discrimination, as soon as they begin to experience it?
If this correct, we can probably expect that as this grouping continues to age, they will also continue to assess their experiences of health care, aged care, social and economic participation and much more through that same lens of fairness, equity and human rights.
In our polling however, there was one area in which those in their 80s and 90s were more likely to report experiencing ageism. This was in the health care system, either by being denied treatments or by being ignored in communication in favour of speaking instead to a carer.
This insight is critically important for those of us who work with older people in the caring industries. In our survey, this largely uncomplaining group of people have identified an important sphere of their lives in which they feel neglected or demeaned on the basis of their age. This gives us a valuable opportunity to review and, if necessary, to adjust our practices and attitudes in delivery of services and personal interactions with older people.
To support this, EveryAGE Counts (with Brisbane North PHN and the healthy@home consortium) has recently launched Every WORD Counts, a guide to taking the ageism out of aged care. It contains simple tools and practical advice to help aged care staff communicate with older people in ways that respect their rights and support their independence and capacity to retain their autonomy, power and dignity.
The EveryAGE Counts campaign has a range of other useful resources to support you to end ageism in your community, and if you haven’t already done so, don’t forget to take the Pledge and join with others to stand for a world without ageism.
Susan McGrath, Senior Policy Advisor, EveryAGE Counts www.everyagecounts.org.au


The Governing for Reform in Aged Care Program’s most recent webinar, ‘Transforming for an Inclusive Future: Cultural Safety for Aboriginal and/or Torres Strait Islander Elders’, explored what reform in aged care will mean for Aboriginal and Torres Strait Islander Elders who access aged care services.
Sarah Brown, Chief Executive Officer at Purple House, and Ken Markwell, Mununjhali man and former Executive General Manager Indigenous Services at Australian Unity, panelled the rich discussion focusing on how executive leaders and governing body members can best partner with Aboriginal and Torres Strait Islander Elders, their families, carers and communities to strive towards a positive future.
Ken continued the conversation with the Governing for Reform in Aged Care Program, sharing deeper insights into the importance of creating and strengthening culturally safe, inclusive and accessible services.
He shared a powerful story with the team about the Bunya Mountains in southeast Queensland.
“Storytelling is at the heart of Indigenous culture and is how history has been handed down from generation to generation,” said Ken.
“Tribes from across Australia would visit Bunya Mountains every three years to feast on the bunya nuts. The only way to get there was by ‘foot falcon’, so you could imagine the vast distances people would travel to feast on these bunya nuts. It wasn’t just about the feast, there were ceremonies and lore conducted and disputes resolved.
“Importantly, some people couldn’t make this journey, such as the vulnerable and the elderly. The people who stayed to look after them were the strongest warriors and best carers.

“Not the second best, not the third best, it was the best of the best who looked after the most vulnerable as they were the holders of knowledge – they were their revered Elders! Those warriors and carers earnt that right.”
The deep respect being embodied in that story is what continues to be applied in Aboriginal models of care today. These models of care have worked since time immemorial
based on trust, respect, knowledge being earned not learned, and relationships always before transactions.
So, how can executives and governing bodies learn from Aboriginal and Torres Strait Islanders to deliver the appropriate approach to care? Ken has provided three practical tips:

1. Genuine co-design, co-delivery and co-decision alongside Aboriginal and Torres Strait Islander people. Whether that is to review aged care practices or actual care delivery, genuine partnership is so important. Practically, this could mean including Aboriginal people on boards and advisory committees, hiring Aboriginal executives right through to front-line workers, and incorporating Indigenous procurement.
2. Organisations should have a cultural capability framework that continually improves systemic cultural capability across the entire organisation. It is all about cultural capability not competence. It is not binary, it is a continuum, because our knowledge and our learning is lifelong.

3. Make decisions on outcomes, not activities or outputs. We need to understand, measure, report, and make decisions on the impact our actions are having on an Aboriginal person’s life, both negatively and positively.
These outcomes must be informed by customers and community driven by what matters to them not just what is the matter.
Ken believes the Australian aged care sector as a whole can learn many things from Aboriginal models of care but also that Aboriginal people can learn about and benefit from modern technologies and clinical capabilities across the sector. It is mutual respect and understanding that will get us there.

“Our identity informs our entire world view of who we are, our connection to country and to each other and everybody and everything including land, water, animals and plants, to the smallest grain of sand – everything has meaning,” he said.
“It is not one hand clapping, right? It is two hands coming together in a respectful relationship to improve the wellbeing of our Elders.”
To hear more from sector leaders like Ken and be a part of powerful and informative conversations, enrol in the Governing for Reform in Aged Care Program today. Visit the program website to find out more and join your peers in the commitment to enable positive change within the aged care sector and govern for reform.
Shannon Robertson, Governing for Reform in Aged Care Program
Salvatore Virzi is a natural-born storyteller. Looking back over his 95 years of living, he has many stories to share about his life, his experiences and working in Sicily’s Regabulto, one of the most beautiful regions in Italy.
This ability to share his past, his culture and his love of Italy in his own language with Co.As.It. Community Services staff allows him to continue interacting with people with charisma and passion – of which he has plenty!
Co.As.It. is a charitable organisation with a 45-year history of service delivery. It began by supporting people from an Italian background but it soon expanded services to include people from all culturally and linguistically diverse (CALD) backgrounds, assisting them with aged, community and disability support programs that enable them to live a rich and rewarding life.

“The care and respect shown to me by Co.As.It. staff is very important. The food is top quality, and every time I move at the Centre, a care worker is there to support me,” Salvatore says. “I enjoy coming to the social group at Casa Serena in Stafford and being able to connect with people and staff who speak my language.”

With 85 per cent of staff speaking more than one language and covering 51 languages in total, Co.As.It. is proud to be able to support the multicultural community with person-centred care within the appropriate cultural framework of the individual.
Team Leader of Care Staff for the South Region, Ludmila Rodriguez who was born in Venezuela, stresses the advantages of having such an extensive range of bi-lingual workers to support clients.
“We have clients from many different countries with many different life experiences. Our advantage is that we can speak other languages and
precisely understand the clients’ needs,” Ludmila says.

“It is hard to remember and speak a second language when you get older. At Co.As.It., we communicate with our clients in their first language, which is a significant benefit if we wish to capture their needs and wishes accurately and with complete understanding.”
Care Services Coordinator Concetta Suizu, a Brazilian who speaks Portuguese, Italian and English , says efforts are always made to match clients with suitable care staff who are familiar with the client’s language and background.
“Before the implementation of services and in designing the care plan, efforts are made to allocate a specific worker with the language and skills to support the client. The care plan is adjusted along the way if necessary,” she says.
Antonio Frassanito, who is 91, is another client whose first language isn’t English, but at Co.As.It., he feels at home.
“I speak Italian and Spanish. My English isn’t so good, which is not a problem, because they speak my language here. So when I need to walk around a little, have lunch or go the bathroom, I feel there is always someone by my side,” says Antonio, who attends the social groups every week.
High levels of diversity and culturally appropriate activities are planned at the Social Activity Support groups located in five locatoins across Brisbane and Gold Coast. Participants enjoy attending the centres which promote social connectivity, community interaction and for many, a good opportunity to form friendship networks.
At Co.As.It.’s community hub Amici House on the Gold Coast, over 300 people use the facility weekly, doing yoga, exercise classes, art classes, Latin dancing and technology lessons – all with enthusiasm and within a great multicultural environment.
Part of Co.As.It. for eight years, Colombian-born Community Care Worker Samir Rivera says that the multicultural aspect of the organisation avoids miscommunication with the clients and facilitates a more personalised service.
“Speaking the same language helps a lot, as well as having the same cultural background as the client. Therefore, I can establish a direct channel and promptly assist them with their needs.”
“Every day it’s a pleasure because I like what I do. I don’t see it as a job. I’m always smiling because I feel so glad. I can say that I have found my mission in life. I want to finish my working life serving the community.”
Juliano Oliveira, Marketing & Creative Content Officer, Co.As.It. www.coasit.asn.au
“They
Culturally appropriate care can make a world of difference

















































































December 18 is International Migrants Day, recognising the contributions and rights of migrants worldwide. It’s also a day to remind people to work together to ensure migration is a safe and positive experience for all.
The Australian Census 2021 reported 15 per cent of Australia’s homeless population were migrants (arrived in the last five years). That’s more than three times the number of new migrants in the general population.
According to the Housing for the Aged Action Group, older migrants, especially Chinese and Indian, often come to Australia later in life and haven’t been able to buy a house, or have come to live with family and if it hasn’t worked out, they have nowhere to go.
As the new Federal Government scrambles to fix a critical shortage of affordable housing across Australia, it’s important that aged care organisations work to improve access to services and support for people from culturally and linguistically diverse (CALD) backgrounds – to help stop people slipping through the cracks.
Amy Yuen, a Victorian case manager from for-purpose organisation VMCH, sees the issues on the ground and believes more can be done at a grassroots level.
Amy supports 66 seniors who are on a low income and are homeless or at risk of homelessness through the Australian Government’s Assistance with Care and Housing (ACH) program. Thirty per cent of her clients are from CALD backgrounds.
Amy says language barriers, a lack of knowledge in navigating Australian systems and services, and poorer overall
socioeconomic status compared to older Anglo-Australians, are just some of the obstacles.
All rang true for Guanghui (Tony) Huang, who fled China in December 2014 for a better life in Australia. Months later he found himself completely isolated and living in a tiny room in an overcrowded share home, in poor health, with limited finances, no job and no support.

“I was down and even thought I was less than others and forsaken,” Tony, who suffers from depression, said.
When Tony was referred to VMCH through the Migrant Resource Centre, things began to look up.
Amy advocated on Tony’s behalf, collaborating with government departments, the Migrant Information Centre, local council, Salvocare Eastern and the Eastern Emergency Relief Network, to find Tony his own public housing unit, which he moved into in June. She also linked him with home and health care services, and was able to source donated furniture.
For Tony, whose rooming house experience was horrific, it’s been life changing.
“Now I can cook what I really like, read in the house and take a bath every day. Hopefully, after living in the new environment, my health will gradually improve and I will be able to do something good for society, in return for the benefits I have received from the government and for the help from VMCH.”
The Federal Government, as part of its Budget in October, announced a landmark agreement between all levels of government, investors and representatives from the construction sector to tackle the affordable housing shortfall
by building one million new homes over five years. It’s an ‘aspirational’ target, and involves incentivising the construction of cheap housing from 2024.
Amy says, while welcome, it’s only one part of the puzzle for newly arrived migrants.
“We need more community education for health care professionals, and housing support services need to be aware of the vulnerability of new migrants who are socially isolated and need to access the public housing system or affordable housing,” says Amy.


“We also need to make sure that once they are housed, there is enough social, emotional and financial support for people to live happy, healthy and longer lives.
A big part of this is community groups and organisations working together to identify at-risk people and link them with relevant services.
“The government also needs to have close supervision on the owners of rooming houses to ensure they provide sufficient support for new migrants to meet their basic needs.”
Along with supporting older people through its ACH Program, VMCH also provides affordable homes to 436 people aged over 55 in 21 communities, with plans to expand its portfolio.
Cassie Zlonzak, Communications Advisor, VMCH www.vmch.com.auBBus FCPA GAICD







Company Director and Aged Care Specialist Health, Aged and Social Care M: 0411 255 331 E: jennene@enkindle.com.au






MBA, Certified Change Practitioner Company Director and Aged Care and Workforce Specialist M: 0447 242 508 E: tash@enkindle.com.au
www.enkindle.com.au
Pre-purchase the 2023 AMH
FreeStyle Libre 2 system offers up to 14 days of continuous glucose monitoring with optional alarms and no finger pricks.† It consists of a small, discreet sensor worn on the back of the upper arm and scanned with the FreeStyle LibreLink app for a reading to help monitor and manage glucose levels.


Feeling lonely is “the worst bloody feeling in the world” said Shoodoo, an 85-year-old resident of an aged care home that we interviewed in 2017.
Since then, her words have been echoed by many older Australians who participated in our research on loneliness in later life. Loneliness does not affect all older people – those more vulnerable to it tend to live in aged care homes or alone, while dealing with ill health and social circumstances that limit their social connections.
Loneliness is a complex issue, usually defined as a subjective experience related to missing companionship and quality social connections. We feel lonely when we lack meaningful relationships with others. Prolonged loneliness has harmful effects in later life, increasing the risk of dementia and depression, among other health problems.
During the COVID-19 pandemic, we conducted a study with older Victorians (aged over 65) living alone throughout lockdowns. These participants already felt lonely before the pandemic. Through 32 diaries and interviews, they shared their lived experiences of loneliness.
We wanted to better understand not only what loneliness meant to them, but also what they felt and how they dealt with it.
Not surprisingly, all described the negative impact of loneliness, from the immense emotional pain that it entails to how it affects their identity and who they are as human beings. The diaries were filled with accounts of despair and sadness.
June, a 73-year-old Victorian living alone with her canary, wrote in her diary that she wished she weren’t here.
Despite all the pain of loneliness, our studies with older people living in aged care homes or alone reach the same conclusion: people prefer to suffer in silence. They prefer not to tell their families, friends or carers that they feel lonely.
the ‘one who has no friends’. It is often associated with poor social skills, even though research shows that lonely older people are as socially skilled as non-lonely people. Secondly, our participants already feel stigmatised because they are old and frail. Admitting to loneliness adds to a degraded sense of who they are.
Lonely older people are constrained by health and social issues limiting their opportunities for meaningful connections, but they are not passive. They still use several strategies to cope with loneliness. The problem is that most strategies are based on concealment or avoidance.
They conceal their feelings because of stigma or because they were previously dismissed when talking about loneliness. They employ avoidance by engaging in activities, such as reading or watching TV, to distract themselves from their feelings. Yet these activities do not help address loneliness; they just mask it.
So, what can we do about it?
In addition to broader initiatives to create awareness and destigmatise loneliness, we can all play a role in tackling this damaging phenomenon. Our participants note that what really helps alleviate loneliness is being included in activities that match their interests and that create opportunities for deep connections – beyond the ‘one-size-fits-all’ model sometimes used in aged care or community programs.

Ensuring that those activities make older people feel valued is also essential. Other simple things can be extremely helpful too, like having someone to ‘just listen’ – not to judge or admonish them, not to tell them to be more resilient or positive, but to listen intently as if they ‘really matter’, as explained by Shoodoo.
Dr Barbara Barbosa Neves (PhD, FRSA), Senior Lecturer in Sociology, Monash University ‘Pandemic diaries: lived experiences of loneliness, loss, and hope among older adults during COVID-19’ was published in The Gerontologist 22 July 2022
This silent suffering happens for two main reasons. Firstly, loneliness is stigmatising since it is seen in our society as an individual’s fault for their lack of friendships. No one wants to be One of June’s diary entries during COVID-19 lockdown. Image credit: The Gerontologist.
An innovative program that aims to improve older Australians’ digital skills by connecting them with student mentors has now launched across the country.


Developed by the eSafety Commissioner, Australia’s independent regulator for online safety, the intergenerational Young Mentors program brings teenagers together with older Australians to share digital skills and knowledge, and help them gain the confidence they need to navigate the online world safely.
“Technology has a wonderful ability to connect, enable and empower individuals, and the importance of this connection was made even more evident during the COVID-19 pandemic,” eSafety Commissioner Julie Inman Grant said.
“For those of us who use digital technology as an essential part of our daily lives, we may not realise how novel it can be to older people who have lived much of their lives without it.
“It’s difficult for anyone to stay on top of the continually evolving digital landscape as new technologies emerge. Ensuring we don’t leave older Australians behind as society continues to move online is essential.”
Young Mentors is a free program that helps community organisations and groups partner with secondary schools to coordinate one-on-one digital mentoring sessions. The weekly one-hour sessions focus specifically on the needs of the older learners and are delivered over a period of six weeks.
eSafety research shows younger Australians are keen to help older relatives get online, with young people more likely to show an older family member how to use technology (59 per cent) rather than doing the task for them when asked (40 per cent).
For older Australians, the program is intended to build confidence in using digital technology, which can create a greater sense of independence, provide greater access to services and reduce feelings of loneliness and isolation.
Young people also benefit from taking part in the program by developing teaching and leadership skills. And people of all ages taking part in the pilot reported increased social connection and understanding across generations.
Following a successful pilot, eSafety is now calling on libraries, councils, aged care homes, community groups and schools to get involved.
“Young Mentors provides an opportunity for genuine connection between generations as we work together to improve digital literacy in Australia, ensuring older Australians can stay connected with family, friends and their communities and empowering younger Australians through a leadership role as digital mentors,” said Ms Inman Grant.
Young Mentors is the latest offering in the Be Connected program, an Australian Government initiative that supports older Australians to access digital technology and online services.

Be Connected is implemented in partnership by the Department of Social Services, eSafety and Good Things Foundation Australia to improve the online confidence, skills and safety of older Australians.
The Be Connected website, managed by eSafety, offers hundreds of resources – including self-paced courses, online presentations, articles, podcasts, and even a games and skills practice area – to help older Australians and those who support them to keep their online skills sharp and increase their confidence using the internet and digital devices. Best of all, they’re all free: beconnected.esafety.gov.au.
“The Be Connected program continues to play an important part in helping eSafety improve the digital literacy of older Australians and make the online world a safer, more positive place for us all to enjoy, and we encourage aged care providers to register for this opportunity,” said Ms Inman Grant.
eSafety Commissioner esafety.gov.au/beconnectedyoungmentors
Sixty-year-old Glenys recently made the move from a Southern Cross Care (NSW & ACT) residential aged care home into a Hume group home in Western Sydney after more than 20 years living in aged care, following severe injuries sustained when she was hit by a car.
“The change in Glenys has been nothing short of amazing,” says Steve Davies, Glenys’ life-long family friend. “Glenys is more alert, her medication has been reduced and she is now benefiting from more one-on-one time with her support workers and has better quality of life.”
There are an estimated 3,400 younger Australians like Glenys living in residential aged care across Australia.
Following the Royal Commission into Aged Care Quality and Safety interim report, the Australian Government announced Younger People in Residential Aged Care (YPIRAC) targets to assist younger people to move out of residential aged care homes and into the community.
As a result, many aged care providers are now working against the clock to meet mandated targets that include: no people under the age of 65 entering residential aged care by 2022; no people under the age of 45 living in residential aged care by 2022; and no people under the age of 65 living in residential aged care by 2025.
With aged care providers and families struggling to navigate alternative, age-appropriate accommodation options for NDIS participants, Hume Community Housing and Northcott Disability Service are providing support.
“We know there is a degree of complexity in understanding the NDIS and what supports are available to assist, so that’s where we step in,” says Scott McPhillips, Senior Manager, Housing for People with Disability at Hume. “We are working with providers including Baptist Care to implement the YPIRAC Strategy.”
Aged care services must support informed choice for a younger person in, or at risk of entering, residential aged care through:
■ deliberative discussions with the younger person, their family, carers and/or supporters to explore age-appropriate alternatives to residential aged care
■ providing up-to-date information on accommodation options and supports
■ ongoing exploration of accommodation and support goals and options
■ noting choice is not considered final and is periodically reviewed through ongoing discussions with the younger person, their family, carers and/or supporters.
Aged care providers must support residents who are NDIS participants and who want to move out, as well as provide younger people with information about how to connect with home and independent living options to ensure they avoid entering residential aged care wherever possible.

Aged care providers must also consider implementing changes in terms of their governance and operations specifically around the support offered to any eligible residents.

Should an NDIS participant wish to find alternative accommodation, the aged care provider must help them to explore alternative home and living options by:
■ asking about their home and living goals
■ directing them and their family to the NDIA website for information about their options
■ encouraging them to contact their support coordinator or the NDIA on 1800 800 110 to talk about their home and living options.
If the NDIS participant does not want to leave their residential aged care or has no goal to leave written into in their NDIS plan, the aged care provider must continue to provide support.
Younger people living in residential aged care, including NDIS participants, are protected by the security of tenure provisions in the Aged Care Act 1997
It’s important to note that aged care operators with NDIS customers may be required to register with the NDIS Quality and Safeguards Commission.
The NDIA will continue to provide support for NDIS participants who choose to remain in residential aged care.
Aged care providers can access the following support to help meet the needs of eligible residents:
■ for help moving young people from aged care to ageappropriate services, email the Department of Health health.ypirac@health.gov.au
■ to get in touch with the Specialist YPIRAC Team that supports NDIS participants to identify an alternative home and living goal, email the NDIS aged.care.advisory.team@ ndis.gov.au
■ for more information and to view the YPIRAC Strategy and Fact Sheets visit www.health.gov.au/initiatives-andprograms/younger-people-in-residential-aged-carepriorities-for-action
Renee Marshall, Disability Housing Engagement Coordinator, Hume Community Housing www.humehousing.com.au
The demand for quality in-home care is rising and the lack of workforce to meet that demand is the biggest challenge home care providers face.
Nationwide, the number of Australians aged 65 and over accessing home care services more than doubled to 140,000 in June 2020, from about 62,000 in 2016 (National Aged Care Data Clearinghouse, NACDC, 2020)
As baby boomers age that demand will surge, with the majority expected to want to stay in their own homes.
There is a deep need for reform to the home care industry, we need a full workforce strategy to address lack of skills, lack of prestige and lack of value associated with aged care work and ultimately help restore dignity to ageing Australians.

Aged care, and in-home care, is highly valued work – we must ensure this is understood and training is provided to keep workers skilled and engaged.
When attracting, recruiting, onboarding and retaining team members, the whole experience must be considered, and communications should be strong and constant.
As an industry, we also need to consider the skills that our workforce will need in the next five to 10 years. For example, ensuring that we incorporate soft skills such as emotional intelligence into our training, to be prepared for the increasing complexity of care needs.
Quality training must remain a top priority of the home care reform agenda to support the continuance of high quality, relationship-based services to clients.
Empowering caregivers of all ages to upskill is critical to strengthening and maintaining the aged care workforce and we’ve taken steps to address this with the recent opening of our Registered Training Organisation (RTO), the Home Instead Academy.
We provide training and support on the job and additionally, caregivers can study a Certificate III in Individual Support through the Home Instead Academy. The certificate centres on home care rather than residential care and builds the practical knowledge and confidence needed to provide high-quality services.
Workforce shortages can also be addressed by tapping into the ‘silver economy’ – older Australians who have valuable ‘lived experience’, are driven to give back and want to work more hours.
In 2020/21, Australians aged 65 and over had a workforce participation rate of 14.8 per cent, compared with 6.0 per
cent in 2000/01. Recent National Seniors research shows one in five pensioners want to get back into work, which is unsurprising, given the increasing cost of living pressures.
With nearly 10 per cent of Home Instead’s 4,300 caregivers aged 65 and over, we will continue to actively encourage the government to make it easier for those of pension age to work for longer and for more hours, if they wish.
Many older Australians report health benefits from remaining in the workforce – it helps them stay physically and mentally active, while reducing feelings of loneliness, isolation and diminishing self-worth.
Our older caregivers are attracted to a role with Home Instead Australia because they are looking for purpose and a way to give back, while also gaining extra income to top up their retirement earnings.
In their roles, our older caregivers excel in relationship-based care. They report that when they walk into the homes of people they care for, there is an immediate connection. They are often of a similar age and there is that empathy, kinship and understanding, which all translates to a good experience.
Going into someone’s home to care for them is a very personal thing. Focusing on and enriching that relationshipbased model is paramount to restoring that dignity for older Australians.
Perceptions that working in aged care is un-glamorous exist, but this is far from the truth – it is meaningful and vital work.
It is up to all of us to change the language we use. If the conversation is more positive, carers may feel more valued, leading to a corresponding shift in long-term retention.
We must redirect the conversation regarding the importance of aged care work; people who do these jobs are often unsung heroes.
Georgia Downes, Chief Operating Officer, Home Instead www.homeinstead.com
ELDAC is your free guide to meeting palliative care needs for your home care clients. A free educational video series is available focusing on key aspects to improve your practice and systematic approach to palliative care and advance care planning. The 6 modules in the video series accompany the resources available in the ELDAC Home Care Toolkit and include:






The way we work and what we consider important has changed dramatically in the past few years.
Not only has distance and isolation forced us to re-evaluate what matters most, but the navigation of a global health crisis has further highlighted the vulnerabilities of our most senior Australians, in turn putting relentless pressure on our aged care system.
We know that older Australians live longer, happier lives at home so long as they remain connected. At Five Good Friends, our sole focus is on ensuring our seniors live vibrantly in their own surroundings, connected to the friends and communities they are most familiar with, for as long as possible.
Our team at Five Good Friends handles home care differently – there are no uniforms, we provide our staff with intuitive reporting technology, and our ‘helpers’ (we like to call them ‘professional friends’) are afforded choices, flexibility, transparency and all the support they need to do what is one of the most valued jobs around.
Unfortunately, there has long been a stigma associated with home and aged care. But it is not all bathing and nursing, in fact a lot of it is about assisting with odd jobs, doing the shopping, driving to and from appointments, and above all else, friendship.
I know the young people of today often get a bad rap for their so-called lack of commitment and waning interested in anything but themselves, but at Five Good Friends we know young Australians have a lot to give and benefit from ‘real connection’ as much our seniors do.
We’re seeing a shift, an increasing number of young people, some of them students, have joined us and many love it so much that they have considered throwing in their studies and opting into home care full-time.
The obvious question is why? All humans yearn for social interaction, and for many Aussies in their 20s and 30s, lending a hand and forming a ‘professional friendship’ with an elderly member of our society is a bit like spending time with and assisting a grandparent and at a time when family means more than it has in years.
Young people across the globe are seeking greater purpose in their work, and it is this flight to purpose, that positions home care as the ideal industry for young people to have fulfilling careers.
Brisbane-based helper Lauren is one such example. Not only does the 25-year-old Occupational Therapy student
earn practical experience on the job, but she also enjoys nothing more than chatting or mastering her Sudoku skills with Richard, who is in his 80s and lives alone in the house he has owned for 50 years.
Such is her passion for the job, Lauren meets another of her ‘members’ Keith once a week for dinner and is just a phone call away should either Richard or Keith need her outside of her regular paid hours with them.
“I couldn’t live at home without her, and besides the help she gives me, I really enjoy her company,” says Richard.
Sentiments like these from our care recipients are not isolated, and while the human element of home care work is a huge part of the appeal, our Lookout technology platform is our biggest point of difference and another drawcard for young tech savvy minds.
Innovative platforms will bring about the crucial change the industry so badly needs it – even the Royal Commission said so.
Lookout is the revolutionary technology Five Good Friends developed and have made available to any home care provider; a home care technology that has been built by a care organisation for care organisations.

To date, the home care industry has been starved of accessible software solutions that meet the needs of its staff and clients. Lookout gives helpers and care recipient’s families transparent access to reports and notes on their loved ones.
And, even more importantly, built-in algorithms detect risks and concerns by analysing the notes entered inputted by the support workers.
Embracing and using the best in technology is also fundamental to attracting the best employees. It streamlines reporting, it makes workers feel more empowered, in control and safer.
Our younger helpers have grown up with technology and adopt it with ease, and for others, it makes their job easier. Our industry doesn’t need to reinvent the wheel, but we do need to redesign it.
If the problem for the home care sector is to attract younger or more high-calibre people, then supporting them to make friendships with older people, with the use of good technology, could be a solution.
Nathan Betteridge, Co-Founder and Chief Operating Officer, Five Good Friends www.fivegoodfriends.com.au
It’s all about creating connections and using the right technologyL- R: Five Good Friends Co-Founders Simon Lockyer and Nathan Betteridge.

I have been in aged care for around five years now, commencing my career as a carer and then moving onto an allocation coordinator, a rostering coordinator, and finally to a social support coordinator.

What I love the most about my career in this field is the fact that I see the effects of what I do every day.
It’s usually the simple little things that matter most. Whether it’s patiently listening to the story behind a family photo, staying for a few extra minutes to chat and laugh, or taking some time to learn about someone – the happy faces in front of me light up my world.
Working in aged care also allows me to interact on a daily basis with seniors who have a lifetime of experience and knowledge. This is a blessing and provides me with plenty of wisdom.
A career in aged care is sometimes challenging, for different reasons, but undoubtedly, we are here to work for human beings, and it is very easy to go the extra mile for someone else.
An extended conversation even after finalising the tasks with the seniors means the world to them, they understand and appreciate these ‘extra miles’ you go for them, and this is instantly reflected on their faces.
I always remember the conversation that I had with a retired doctor who was one of our seniors. He has given me a lot of advice and was like a father or grandfather figure to me. Although we were always told to keep a professional boundary with our clients, this client, in particular, is always in my heart. I lost my dad when I was nine but working in aged care lets you gain a lot of ‘dads’.

My current role as a social support coordinator involves coordinating and planning seniors’ outings and gatherings and has made unforgettable memories with our seniors. We took them out bowling and to the zoo. These fun times and memories are what I treasure most in this career, and it makes this job so rewarding.
To improve somebody else’s life is the reason why people chose to work in aged care, and we can see the effects of these improvements immediately. I honestly think this is what makes aged care very special; you get to see the result of your work instantly on the faces of our lovely seniors.
When I talk to my friends about their jobs, they always complain about the people they work with, but in aged care, because you really can’t do the job unless you’re very kind, patient and positive, you will always deal with the best people.
Aged Carehumansofagedcare.com.au

Aged care workers are used to going the extra mile to support their older clients, working hard to ensure they can remain independent in their own homes with access to important health and personal care needs.
This dedication has been put to the test across Australia during fires, floods and COVID-19, with aged care workers continuing to rise above despite finding themselves in need of support.

During the recent devastating floods in Victoria, for-purpose organisation VMCH’s At-Home Aged Care (AHAC) staff living in flood ravaged areas banded together to support each other through the crisis, and ensure hundreds of older residents across the Hume region remained safe and well.

Many Victorian towns remained on high flood alert for extended periods, as the state experienced some of the worst floods in its history.

When danger peaked for Shepparton resident and Rostering Coordinator Brooke Chew, her colleague, Clinical Case Manager Eloise Crees, stepped up. Eloise and her husband were on the road at the time, testing out their new caravan with a trip to Echuca. But the trip was short-lived, with the pair turning around once they heard of flood levels in Shepparton, a short drive from their property in Yabba North.
“I knew Brooke lived alone so we wanted to help,” Eloise said. Her instincts were right. Emergency Services warned Brooke to evacuate before it was too late.
The trio did what they could to protect Brooke’s home, driving to the nearby showgrounds to line up for sandbags, which they took back to Brooke’s to help protect her home. Thankfully, the water only reached Brooke’s letterbox, but the whole experience was deeply unsettling.
“I’m ok now, because I know, at the moment, my house is ok,” Brooke said. “I’ve been very up and down all week but having the support of Eloise and her family has been great. The caravan was like a luxury. I would have been happy sleeping in a tent or on Eloise’s driveway at one point! It was a difficult situation.”
The pair’s next priority was to ensure they were set up to help their older clients. VMCH provides help at home to more than 1,400 people across Victoria with home care, including domestic assistance, house and garden maintenance, and allied health support. Many of them live in the towns hardest hit by the floods, including Echuca, Rochestor and Shepparton.
Eloise set Brooke up in her study, and she took the dining room table. The pair got to work, coordinating client rosters and working alongside case managers and client liaison officers to make welfare checks on VMCH clients to ensure they were safe and had adequate food and medications.
They are quick to point out they’re not the only ones who helped out, with most AHAC staff across doing extra to support hundreds of clients affected by the floods.
“One of our colleagues’ houses was completely flooded, others were trapped in their homes, and everyone was dealing with road closures, power outages and evacuations,” Eloise said. “Being involved in a natural disaster is a pretty terrifying thing to happen to your community, and especially being elderly and vulnerable, we just wanted to help them.”
VMCH CEO Sonya Smart described the actions of Eloise, Brooke and their colleagues as “courageous and resilient”.
“Their stories of support for each other and clients has provided VMCH with a sense of pride and renewed optimism, as they have shown the rest of us the importance of being good neighbours, friends and colleagues.”
VMCH Home Care Programs Manager Magali Kaplan said she was “extremely proud” of her colleagues.
“Most people wouldn’t be able to conceive of working during such a time, but our staff stepped up and put their own challenges aside to ensure the people we support are looked after,” she said. “It’s incredible.”
www.vmch.com.au




As the aged care industry continues to grapple with staff shortages, increased competition, and growing compliance and regulation pressures, workers find themselves with less time to spend with residents. Aged care workers have faced an extremely difficult few years, and chronic understaffing and increased reporting requirements have only made it more challenging to deliver the high levels of care they aspire to provide.
Regardless of staffing levels and quality of care aspirations, aged care workers must still complete a significant amount of administrative work before they can clock off from their shifts. This can lead to low morale, burnout and even higher levels of staff turnover, compounding the unresolved issues.
Meanwhile, compliance requirements, including the recent introduction of the AN-ACC care funding model, are not just tightening, but also changing often. Upholding compliance is becoming increasingly complex and continues to remain an overwhelming task for aged care providers. This is due to reporting requirements that are not a one-size-fits-all approach, as each organisation needs a solution that can fit their specific needs and systems.
One way that aged care providers can improve the employee experience, free up staff workload to spend more time with residents and streamline operations, is by removing the burden of disparate, inefficient administrative systems.
Centralised, modern workforce management (WFM) solutions can help aged care providers maximise resources and cope much more effectively with staff shortages, increasing operational costs, compliance changes and rising competition.
A holistic suite of people solutions including WFM, human capital management (HCM), and payroll automation enable aged care providers to improve the way they manage time and attendance, scheduling, absence management, human resources, hiring and labour analytics.
A modern WFM solution allows aged care providers to:

■ create optimum staff-to-resident ratios for superior and value-based care experiences
■ retain staff through fair and consistent application of leave, rostering and other policies
■ reduce costs through increased visibility into potential issues, solving them sooner
■ achieve compliance through proactive tracking of credentials, licences and regulations
■ increase staff empowerment through intuitive and easy-touse tools that deliver flexibility.
It’s important to roll out solutions in a thoughtful and methodical manner that includes proactive change management, training and an ongoing support strategy. Once staff can see the benefits to the change, it will be easy to get everyone on board.
It can also help to choose a WFM solution provider that supports aged care providers with a team of healthcare experts; a partner that can evolve with aged care providers as the industry continues to change is essential.
UKG worked with Australian Unity to correct issues around accurate pay and staff experience. By providing a unified platform and a single source of truth, UKG helped Australian Unity pay employees accurately and efficiently, saving approximately 90 hours per fortnight. The insights provided through the platform empowered Australian Unity to futureproof its workforce management strategy. And, the self-service capability in the system meant that workers could see open shifts, request time off or preferred shifts, and importantly, focus on residents with more time for care.
Another community services provider also implemented UKG’s WFM platform to elevate its employee experience and improve process efficiency. Employees can now see at a glance their working hours and a pay breakdown. Rather than using paper-based timesheets, the organisation now uses mobile apps and desktop computers to let people clock in and out, which delivers accurate and reliable data, in turn improving its compliance capabilities. The organisation also minimised manual administrative time due to automated workflows within UKG, which meant more time could be dedicated to resident care.
Choosing people-focused solutions rather than a finance focused approach can help lead to higher employee engagement, improved organisational culture and decreased levels of burnout – helping you provide the highest level of care and stand out from the rest as an employer of choice.
Darren Kilmartin, Director of Healthcare, UKG www.ukg.com.au/industry-solutions/aged-care
Removing the burden of inefficient administrative systems to create a better experience for everyone
IT Integrity provides technology consultancy and solutions that leverage existing investments and achieve business outcomes.
A robust consultative capability designed and scalable to suit your organisational needs.

A comprehensive set of governance frameworks to ensure technology opportunities and considerations empower your organisation.
Comprehensive capability across system integration, application development and organisational change management.
Managed services offering complete and hybrid solution support models. We’ll look after your systems so you can focus on running your business.
Find out more at itintegrity.com.au
Workforce challenges are impacting all care sectors significantly, in particular, aged care. On top of structural weaknesses in the labour market, care organisations have struggled to hire staff and fill rosters due to COVID-19 sicknesses, close contact regulations, lockdowns and border closures. Additionally, care work is demanding, relentless and poorly remunerated.
Maybe the national wage case and migration policy changes might alleviate some of these problems. But the fact remains that the care sectors will have to find better ways to solve their own problems.
Let’s start by dragging recruitment, roster filling and on-boarding processes into the twenty-first century. We must embrace modern technology to utilise the power of social media, digital marketing and artificial intelligence to simplify and accelerate the antiquated manual processes many organisations still use.
Coming from an Asian background where respect for elders is paramount, I originally planned to develop an aged care facility. In familiarising myself with the sector and its needs, I realised that
the aged care labour market required a more urgent fix than bed shortages.
I could see that providers were looking for workers and workers were looking for providers, but both parties were stumbling around in the dark.
From CareBridge’s experience, we have found that by using multiple channels and sophisticated digital campaigns, it is possible to unearth more active and passive jobseekers than we traditionally thought possible.
Then by creating a worker clearing house, it is possible to qualify and vet jobseekers to create a willing and eligible candidate pool. Candidates appreciate this because they don’t need to submit multiple applications to different employers for different roles nor do they have to prove their eligibility to work, police check, work right, vaccination status and so on, every time.
The next critical mechanism is to enable providers and candidates to find a great match easily. This is where artificial intelligence (AI) comes in – to partner the most suitable candidate with the job that fits them best. Since AI learns and improves its connecting capability, the matching process becomes increasingly accurate.

The next transformation is to grab available candidates quick smart. Typically, the sector has too many steps
in its recruitment process. Often by the time shortlisitng is complete and candidates are selected for interview, they have found another job.
By contrast, technology can recommend candidates for interview literally overnight. We find that the candidate experience and hiring conversion are equally as important as attracting applicants, and that we are often overlooking this critical element.
Then in an integrated system, interviews can take place, references can be checked, job offers made, employment contracts signed and new staff onboarded, all of this done digitally and automatically.
Using modern technology, HR professionals use the skills they trained for – to choose the best candidates –rather than spend their time in manual processing.
There are more workers to recruit if we are creative in how we find them. If we use technology appropriately, we can more efficiently find the right candidates. If we automate our processes we can jump faster to secure the people we want.
No workers to hire or can’t we find them?
Evan Wang, Director, CareBridge www.carebridge.com.au
The aged services industry is on a massive journey of transformation that has compelled aged care providers to focus on a range of improvements in delivery, workforce transformation and culture change.


As the aged care industry workforce transforms, the balance of aged care workers (now defined as ‘Personal Care Workers’) will transition from on-site facilities and the numbers of PCW employees will significantly increase in the home care sector.
Currently, the Home Care Workforce Support Program is supporting the aged care sector to grow the home care workforce by 13,000 workers over the next two years. These numbers will significantly increase over the coming decades in line with projected increases in demand for high quality home care versus residential care.
Traditionally aged care workers have worked in a controlled environment. On-site, within a service provider’s facility where work health and safety risk management can be more easily identified, managed and monitored directly.
The increase of in-home work in aged care means the potential for a greater number of workplace risks and injuries occurring ‘out in the field’ or in the home of the client.
Standard 7(3) (d) of the Aged Care Quality Standards states: The workforce is recruited, trained, equipped and supported to deliver the outcomes required by the Standards
This standard has reinforced the firm responsibility on a service delivery organisation to ensure that training provided not only encompasses the development of technical skills and knowledge of the job, but also the capability to keep workers safe.
The key to complying with the Standards is to train workers to identify and manage the most common risk areas in a home care work environment.
■ Slips, trips & falls. The most common injuries in home care result from unnoticed obstacles, loss of balance, slippery floors, loose mats or aged carpets and floor surfaces, and electrical leads.
■ Manual tasks. Transferring, showering or dressing clients, moving furniture, sudden force or movement by client, prolonged or awkward posture, and low bed heights can result in musculoskeletal health issues.
■ Electrical hazards. Overloaded powerboards, or aged, faulty or damaged electrical household items, can be hazardous.
■ Hazardous substances or chemicals. Cleaning hazardous substances or using hazardous cleaning chemicals in small
or poorly ventilated areas, or gardening with poisonous chemicals and sprays, can pose a risk to health, particularly as they may contain allergens.
■ Biological hazards. There are infection risks, such as from COVID-19, allergies, contact with blood and body substances, handling and disposing of clinical waste, soiled laundry, and contact with animals. Chicken pox and rubella risks pose a particular danger to pregnant women.
■ Workplace stress. Stress responses can occur when a worker doesn’t feel they are coping with the role, environment or relationships with others. This may include excessive demands by clients or managers, working alone or in isolation, emotional attachment to the terminally ill, client dissatisfaction feedback, and excessively tight schedules.
■ Work-related violence. Violence at work can be related to changes in clients’ behaviour due to a medical condition, e.g. dementia; exposure to an aggressive family member, resulting in verbal abuse, physical slap, hit, kick, hair pull, spitting and scratching; a thrown object; or clients’ pet attack, bite or scratch.
■ Driving risks. Managing client behaviour while driving, poor weather or road conditions, rushing due to client delays or tight scheduling of work.
Developing a framework of risks and controls around these key areas and ensuring PCWs are effectively inducted and trained for roles in home care – in the identification, application of risk reduction controls, and documentation and reporting – to ensure they are equipped to safely manage their environment.
Michael Martin, Certified Chair, Safety Champion, Managing Director & Coach, Proven Safety Solutionswww.provensafetysolutions.com.au
Contact:
www.throne.com.au
The functions of the ‘Standard’, ‘Splayed’ and ‘Fold Down’ rails have been incorporated into the ‘3-in-1’, making it the most convenient toilet support system on the market. The benefits of the Throne Accessories ‘3-in-1’ Rail System include:

This rail replaces the previous three models
Simplified ordering... etc
The Throne Spacer has been developed to add height without changing the appearance of a standard toilet and toilet seat, and offers comfort and safety.






This particular Bariatric Rail model meets the needs of the larger built person. The handgrips are supported by adjustable legs that are firmly positioned to the side of the toilet by rubber-capped feet to prevent tripping. The Bariatric model comes in polished stainless steel.

With
Prescribers say...
“eScripts are great!” Dr Victor Tun, GP
“I like eScripts, I think it has reduced chance of medication errors for residents and it has reduced the bureaucracy of sending paper orders to a facility and paper scripts to the pharmacy.” Dr Adel, GP, Blue Care Brassall Village Facilities say...
“The reporting tools are easy to use and the support from MPS has been fantastic. The introduction of eNRMC is a massive benefit to after hours and areas were GP access is limited.” Janet Rhodes, General Manager, Aged Care Services

“The support from the MPS Connect team has been invaluable with regards to educating GPs and staff and providing on floor support has made the transition much easier for all.” Lanna Ramsay, Head of Aged Care, OzCare Pharmacists say...
“The feedback I am getting from doctors is great.” Shi En Ng, Pharmacist, Infinity Pharmacy Kawungan
Hello@MPSConnect.com.au ■ 1800 003 938

“Anyone with a pulse!” This sentence has been echoed across the industry over the past few years as organisations are screaming out for staff.
We are facing one of the biggest staffing shortfalls and have yet to get through the impending summer period, which is notorious for staff annual leave, leaving big gaps in rosters.
It has always been an easy option to use nurse agencies during this time, which is reasonable, though expensive and limited in its service – not knowing the other staff or residents, operational processes and procedures, can create inefficiencies and less than ideal care.
At the same time, the existing staff feel exhausted, stressed and are leaving in masses.
Numerous executives and managers from the industry are reporting the struggle in finding suitable new candidates at most levels of their organisations from Personal Care Workers, support staff (to provide help in the laundry and kitchen) and administration staff.
Some organisations are using any member of staff to assist with basic care needs, when they experience a shortfall.
With time and quality care being stretched to the limit, there may be more clinical issues or other risks. As organisations battle to deliver the fundamentals, older people are the ones who miss out, potentially feeling more isolated and vulnerable.

The large exodus of fatigued staff post COVID-19 and a poor community view of aged care (partly due to some media stories), is making recruitment a real challenge, even with government incentives.
Attracting workers into the industry has always been difficult with limited career progression, inadequate working conditions, and incomparable wages to similar sectors. We need to change the community mindset to entice the next generation of carers.
care workforce growth projections currently show significant concern. CEDA Senior Economist Cassandra Winzar states that “if we continue this growth rate (2 per cent per annum) we would face a shortfall of over 400,000 workers by 2050 against the Royal Commissions proposed minimum standards”. The CEDA’s analysis suggest that annual workforce growth needs to double per annum. We need help now, we need new blood now, we need a pulse now.
New groups of potential staff are now starting to put up their hands to fill the void. Traditional recruitment, training and retention of staff is being redesigned to help fill vacancies, but it is still slow.
While the training and education focus is to enable a practical ‘on the ground’ supported workforce as soon as possible, we need to tread lightly. We cannot drive people through at such a pace unsupported. Retention of staff must be the ultimate long-term goal, not just filling the gap now.
Career pathways and training analysis consultation assists organisations to create a robust skilled workforce which helps to secure long term employee loyalty, and increase skill level across the organisations to address staff shortages in any situation.
The best approach is collaborative, so that we can create strong partnership connections, to build a multifaceted strategic workforce platform across not only the aged care sector but also the disability community sector. At Vative Healthcare, we strive to do this, with our workplace-based training delivering unique solutions to our clients and students, at every level of an organisation.
Find your workforce partner and start building your skilled carer workforce solutions today, so it’s not ‘just a pulse’, but a healthy, educated team.
Carmie Walker, CEO, Vative Healthcare & Nursing Academy www.vativehealthcare.edu.au
With over 235 meals developed by dietitians and prepared by chefs, Lite n’ Easy offers a delicious, food-first approach to promoting independence, choice & health for older Australians.
Lite n’ Easy have also introduced a new range of meals called My Choice which have been designed to meet the specific nutritional needs of older people who may have a reduced appetite. My Choice meals provide the same energy and protein (an essential nutrient for seniors) as our standard dinners but in a smaller portion, making them easier to finish.
Lite n’ Easy partners with many Home Care Package providers across Australia, so that seniors can have access to even more affordable healthy, delicious meals. If eligible, HCP recipients could save 70% off the cost of their meals.



Lite n’ Easy’s service is flexible with no lock-in contracts or subscriptions, so customers are free to order week-to-week as needed.
In addition to supporting HCP providers and recipients, Lite n’ Easy is now also supporting the broader Aged Care sector by providing meals in bulk to respite centres, residential aged care facilities, hospitals and many other organisations looking for alternative healthy meal solutions for their employees and residents.
For an effective and affordable meal solution to suit your business needs, please email Lite n’ Easy at: agedcare@liteneasy.com.au
Visit www.liteneasy.com.au/my-choice or call 13 15 12 for more information.
“It’s given me back my independence. It’s given me back my health. It’s just wonderful.”
“The meals from Lite n’ Easy are a tremendous help for my health and independence - one of the best food delivery services I have tried.”Aunty Barb & her daughter/carer, Yoni Penny - QLD NDIS participant
Dementia is an irreversible, slowly progressing illness and sadly the second leading cause of death in Australian people, and the leading cause of death for women.
There are different types of dementia, including Alzheimer’s disease, vascular dementia, frontotemporal dementia and Lewy body disease. Dementia can be diagnosed in individuals in their 30s, 40s and 50s, but it is more common in people beyond 65 years of age.
This year, Dementia Australia has confirmed there are 487,500 Australians currently living with dementia. Without a medical breakthrough, the number of people diagnosed is expected to increase to almost 1.1 million by 2058.
Preventative measures to exercise the brain and aid brain cell regeneration are effective as part of a healthy lifestyle, and carers who have the right education for best-practice personcentred care can make a big difference. In addition, ensuring that care for those living with dementia effectively transitions into palliative care is vital to maintaining and supporting someone’s quality of life.
More than two-thirds (68.1 per cent) people living in residential aged care homes have moderate to severe memory loss and cognitive impairment.
Over the past decade, there has been increased human rights recognition with the United Nations Convention on the Rights of Persons with Disabilities coming into force. This charter of aged care rights requires people with a disability (including those living with dementia) to enjoy the same rights as everyone else. These rights include autonomy in decision making, independent living and community inclusion, and liberty.
The Aged Care Quality Standards, through reference to dignity, respect, freedom from abuse, choice and independence, support shifts in aged care service provision consistent with human rights.
Almost 1.6 million people in Australia are involved in the care of someone living with dementia. Practical education for all staff working in aged care supports consumers to lead a meaningful life, conduct advance care planning and helps to uphold their rights as valued members of our society and our communities.
Kineo leads the way in health and aged care workplace digital training with several dementia-focused online courses co-created with subject matter experts in health, disability and aged care. Dementia titles align with the Aged Care Quality Standards and provide practical knowledge that can be directly applied in the workplace.
If you oversee workers that provide care to consumers living with dementia, support your people to better understand complexities and how to best support individuals with a person-centred care approach.
As a leader in digital training about dementia care, Kineo courses are a good place to start. Users can take up a free 14-day trial and sample many titles in the health, disability and aged care category including ‘End Stage dementia’ and ‘Dementia and incontinence.’
Across this topic, courses include:
■ What is dementia? Understand what the term means, the impact on a person living with dementia, and the need to provide a person-centred approach to care.

■ Person Centred Care. Learners will develop a deep understanding of what person-centred care means and the knowledge necessary to apply it when caring for people living with dementia.
■ Effective communication. Learn how to practise good, effective communication when caring for someone, including verbal and non-verbal communication.
■ End-stage dementia. The focused training covers: what end stage dementia is and what happens when a person in care enters end stage; how members of your care team can work together to provide an individual, person-centred approach to care; managing and implementing assessment directive and planning; and how to make the right decisions in a very sensitive time for the person in your care.
Sally Tutill, Content and Social Manager, Kineo www.kineo.com.au
Kineo is a leader in digital training for dementia care.

Blue Light Card, the UK’s number one discount provider for frontline workers, has launched in Australia
Australians have seen first-hand the constant strain aged care workers have endured in the last few years, significantly amplified by the pandemic. While workers strive selflessly to provide care to others in environments that are often stressful and difficult, retaining staff has been a challenge, especially in the wake of the COVID-19 pandemic.
With many talented aged care workers choosing to leave the workforce altogether, the Committee for Economic Development of Australia (CEDA) estimates the industry is losing around 65,000 workers each year, while 38 per cent of aged care workers are intending to leave within the next one to five years.
One way to give back to your staff, is by acknowledging their efforts with a discount card for everyday items – to make their lives a little easier.
Blue Light Card is the UK’s major discount provider for frontline workers, and has just launched in Australia, with aged care workers the first in line.
They’re offering all aged care workers best in the market discounts, savings and experiences from top brands and local businesses in the hope that these savings can ease some of the stress. From everyday essentials to adventures with the family, Blue Light Card covers all aspects of living.
Blue Light Card General Manager, Tracey Duff, is immensely proud to work for a purpose-led business that will now be looking out for Australian aged care workers.

“At some point in our lives, we have had a loved one that needed the care of an aged care worker. Each day I come to work, I get to help aged care workers and their families just
as they care for so many. I am so grateful to be a part of a company with such an important purpose,” said Tracey.
“Aged care workers have one of the most important jobs. Without them, our loved ones wouldn’t be in a safe environment. Blue Light Card acknowledges all the hard work and dedication they put into caring for so many. To show gratitude, we are connecting aged care workers with partners who want to give back.
“We want to ensure that aged care workers feel they are a part of a community that is there for them, as they are there for so many.
“Especially with the cost of living increasing, Blue Light Card recognises the challenges staff have endured and we look forward to making the everyday lives of Australian aged care workers a little easier.”
Major brand partners have already signed up, including Adrenaline, Angara, Apple, Banana Republic, Beginning Boutique, Ben Sherman, Boohoo, BoohooMAN, Bugaboo, Check My Body Health, Donner Music, Elite Supps, EveryPlate, Experience Oz, Expedia, Floraly, FOREO, GAP, General Pants, ghd, Glue Store, Happy Skin Co, HelloFresh, icebreaker, Jeanswest, KitchenAid, Lee, LOOKFANTASTIC, Lovehoney, Myprotein Australia, MyRepublic, Nautica, P&O Cruises
Australia, Proviz Sports, Princess Polly, RedBalloon, Simply Sensitivity Checks, Speedo, SurfStitch, The Body Shop, THE ICONIC, Wotif, Wrangler and 2XU.
To become a Blue Light Card member, the cost is $9.95 for a membership that is valid for two years. It could be a fabulous way to acknowledge your team members at Christmas.
Tracey Duff, General Manager Australia, Blue Light Card www.bluelightcard.com.au


Home Instead Sydney North Shore & Northern Beaches recently announced its CAREGiver of the Year 2022 with Linda Chilcote taking out the award.
“Linda’s love of people shines through each day,” said Rose Harney, Home Instead Sydney North Shore & Northern Beaches People Experience Manager.
“She is a caring, empathetic, and genuinely beautiful person. She is dedicated to her clients, caring for them with compassion, anticipating their needs, respecting their diversities, and treating each person with dignity and respect.
“Time and time again she has shown that she makes a fundamental and deeply meaningful difference in the lives of her clients and their families.”
Linda is able to find the perfect balance between remaining professional, while still sharing her heart, helping her build trust with even the most challenging clients.

In the case of a client who was completely resistant to care, Linda provided him with honest, open, practical and proactive care, gently convincing him of the importance to shower regularly. She was respectful of who he was, his history, his story – the true man behind the veil. This enabled her to form a strong bond with the client and a trusting relationship with the family.
By being a reliable and stable presence, she was able to gain his trust and build a rapport, and the client was ultimately happy to accept Linda’s help with all aspects of his care. Through her dedication and perseverance, Linda was able to significantly improve the client’s quality of life and became an integral part to his ability to remain in his own home.
Throughout her life, and particularly during the period of caring for her sister with MS, Linda has understood that it takes more than just one person to care for another. Embodying the philosophy ‘it takes a village to raise a child’, she not only supports her clients, but also their families, friends, health professionals and others who care for them. She adds to her client’s wellbeing by providing Home Instead with invaluable feedback which helps ensure better outcomes, such as hazard identification, the need for aids, any changes in their physical and mental state, and the need for more outings.
Caring for many clients with high needs – ranging from severe dementia, learning difficulties, hoarding and squalor, vision impairment, advanced Parkinson’s, and members of the Culturally and Linguistically Diverse (CALD) community – she always remains professional, non-judgemental and holistic in
her approach, truly embodying what it means to be a Home Instead CAREGiver.
It’s worth acknowledging Linda, not just as an individual but also as a representative of the many unsung heroes working in aged care, who go the extra mile for older Australians, helping them to maintain their independence and improving their quality of life.
Linda Baraciolli, Aged Care Today Editor & Communications Adviser, Aged & Community Care Providers Association www.hisydnorth.com.au
The Final Report of the Royal Commission into Aged Care Quality and Safety emphasised that ‘provider management and governance has a direct relationship with all aspects of care’. Recognising this, the Australian Government has introduced a raft of legislative reforms focused on uplifting the sectors’ approach to governance.
The implications of this are two-fold. Most immediately, there will be new responsibilities for approved providers in relation to the membership of their governing bodies, the establishment of new quality care and consumer advisory bodies and the introduction of a new non-delegable statutory duty to deliver safe, high quality care.
A ‘suitability’ test will require key personnel to have the necessary skills, qualifications and experience to deliver aged care that is safe and high quality.
There is also a new Code of Conduct for the aged care workforce – including directors – and approved providers that will require compliance with increased reporting obligations and annual attestation requirements.
More broadly, these reforms represent shifting expectations from both government and the Aged Care Quality and Safety Commission.
Against this landscape, the Commission is adopting a more robust regulatory posture in their engagement with providers. Recent legislative reforms will also extend the Commission’s investigation and enforcement powers to more closely resemble those held (and exercised) by regulators like the ACCC and ASIC.
National Care Solutions is ready to work with you to achieve maximum outcomes for your residents and business though contemporary ethical methodologies. We deliver online and alternative training & consultancy services.
National Care Solutions is a professional customer focused aged care specialist focusing on management and training for aged and home care providers. NCS specialises in providing assistance for services of all sizes, including rural and regional standalone services.
The sector can expect increased surveillance activity and more frequent and public enforcement action, with potentially serious consequences for aged care workers, key personnel and providers.
While many providers in the sector are focused on compliance with these new obligations, more will be required if providers are to navigate the evolving and ever changing regulatory landscape.
The articulation of a new statutory non-delegable duty of care will bring with it, a significant uplift in the level of individual responsibility of board members.

The Commission will also have strengthened enforcement powers including enforceable undertakings, banning orders, civil penalty provisions and accessorial liability for key personnel.
The reforms will also bring increased transparency regarding the performance of providers.
Approved providers will be required to report details of key personnel and material changes, information on staffing and care minutes, financial information and complaints data. In addition, data from the Serious Incident Response Scheme will be triangulated with new quality performance indicators, consumer experience reports and quality standards, which will inform the new star rating system in residential aged care. This
data will likely also be used by the Commission in undertaking its monitoring and compliance functions.


The governance reforms bring with them a sharpening up around provider governance.


The Department of Health and Aged Care has indicated that providers are expected to take a ‘best practice’ approach to discharging their governance obligations. The Commission have published a range of guidance materials and other resources to assist providers in implementing these reforms.



Providers should formulate a regulatory engagement strategy for responding to the Commission, which should set out clear organisational expectations. Proactive risk management strategies which identify and remediate organisational risks, will be the key to avoiding or responding to regulatory intervention.

It is timely for providers to consider whether their current systems of reporting and record-keeping adequately meet the demands of the new regulatory landscape, including the need to consider and respond to information requests from the Commission in a short period of time.
Review of these processes will also enable providers to consider whether information flows to the board and executive remain ‘fit for purpose’ and are operating effectively.

Penelope Eden, Partner, Minter Ellison www.minterellison.com

The last couple of years have been very challenging for the Aged Care sector and the need for change is not going away. In fact it is likely to become even greater.


At Realise Performance we strongly advocate that organisation’s must take control of their own destiny to make sure they are well positioned to maximise their future.
An important first step in realising these ambitions is to establish a highly competent, high performing leadership team encompassing both the Board and the Executive Leadership.
Realise Performance works with organisations to help Board and Executive teams through a range of renewal processes designed to strategically reposition individual organisations.
To find out more about how we can help call me on 0412 884 865 or send me an email chris@realiseperformance.com.au

www.realiseperformance.com.au
www.healthstaffingaustralia.com.au info@healthstaffingaustralia.com.au

Governance structures and mechanisms underpin effective service delivery and in turn deliver safe, quality care; they are the cornerstone of consumer outcomes.
Good governance is not just an objective in itself, rather, it establishes the framework for decision making and determines the allocation and prioritisation of resources to deliver care.
Governance is also a crucial element of the leadership, values, culture and change needed through reform and transformation, by connecting the board and executive oversight roles to the performance of frontline workers and the rest of the organisation.

Why does governance needs to change?
In addition to constant pressures and disruption, the public, consumers and family members have contributed to increased expectation and demand for services at an unprecedented pace, creating the need to reflect on the relevance and effectiveness of governance skills, structures and processes needed for effective and responsive decision making and oversight from ‘the bedside to the board’.
Which questions should you be asking?
Governance structures, processes and behaviours within an aged care organisation should foster a consumer and purpose-led focus, and the board should get assurance that services provided are of high quality in accordance with consumer and public expectations.
In order to gather this information, boards should start with three key questions:
1. Where are we in terms of achieving our purpose? What is our north star? Reflect on how often the
governing body revisits this question, and the extent to which ‘purpose’ is explicitly brought into monitoring, oversight, consumer engagement and decision making.
2. How do we know our service is providing the quality of care that older Australians expect and deserve? Reflect on the key metrics and data sources (beyond what management is reporting) that the governing body seeks or receives.
3. How prepared are we as an organisation, to respond to the changing needs and preferences of consumers, and upcoming reforms? Reflect on your organisation’s readiness, appetite and capacity for change. Consider the barriers that might exist and the cultural shifts that may be required across the organisation to enable it to be more aware, responsive, agile and ready to manage changes.
Answering these questions may require actions that fundamentally change the way governing bodies and executives currently lead and operate. While change can be confronting, it is achievable through structural shifts and an openness to improve.
The structural shifts required include revisiting accountabilities and obligations to ensure that the focus of governing bodies is equally balanced on compliance and performance outcomes.
Governing bodies may wish to consider the following:
■ Revisit the purpose and composition of committees. In doing so, consider how the voice of consumers is being brought to the forefront of the discussion and decision making.
■ Plan ahead. Ensure that your strategy has a three to five year horizon that includes some ‘scenario testing’
of different social, environmental and governance related trends. This should be informed by regular updates from external sources, consultants and experts to stay informed of sector trends.
■ Assess the effectiveness and maturity of your risk frameworks. Ensure your risk mitigation strategy focuses on strategic, macro risks that can often be outside the organisation’s control, and are not focused purely on compliance requirements.
■ Restructure board and committee papers. Ensure that there is clear alignment of papers to compliance and performance objectives.
■ Review governing body processes knowledge and skills. Ensure that your governance processes are based around the needs of consumers with a deep understanding of the system, including the complexities, risks, service needs, funding, data and disclosure of information. Put in place development plans and succession plans to fill any gaps over time.
Governance is not a ‘one-size-fits-all’ solution. It is fundamentally, how an organisation organises itself to ensure that it fulfills its purpose in a viable, sustainable and ethical manner. In the aged care sector, the solution is dynamic, and ‘getting it right’ is a journey rather than a destination that requires ongoing iteration and continuous improvement.
Governing structures, processes and skills need to evolve in line with the external context, new reforms, emerging risks and the needs of consumers –ensuring providers and governing bodies consistently place older Australians at the centre of everything they do.
Claire Richards, KPMG Partner Health, Ageing & Human Services | Audit, Assurance and Risk Consulting; Susan Staples, KPMG Director Health, Ageing & Human Services | Governance; Nicki Doyle, KPMG Partner National Sector Lead | Ageing www.home.kpmg
Clinical governance in its simplest form is ensuring all elements of your operation create a safeguarding net around your consumers.
Each area of operations – clinical care, progress notes, reviews, rostering and clinical supervision – is like a slice of Swiss cheese. A hole here and there is not an obvious problem as a risk may not escape because it is being blocked by the next slice of operations, but where holes in your system line up, there is potential for the consumer’s clinical safety to slip through all the layers.
These holes in your clinical governance, small and large, is what the Aged Care Quality and Safety Commission looks for during a quality review and though each service makes its own unique errors or ‘holes’, the unifying factor is that each service typically has lost sight of, or has been unable to manage, the small things which play into a greater risk.
Due to the reality of complex service provision, the Commission looks closely at how the aged care service identifies and manages risks associated with their consumers, workforce and services.
Frequently, services fail in clinical care not because of ambivalence but because they have simply not realised there was a risk. This is why strong clinical governance is more than systems. There must also be a strong cultural and behavioural element where everyone has confidence because the team has had the right training and has been given the right tools, and there’s an organisation-wide approach that provides support.
This broader view of the importance of strong clinical governance is brought into sharp focus when we see the impact a failure of clinical care has staff morale, confidence in themselves and each other, and the reputation of the service.
Balancing choice and risk and clinical governance is always a challenge when we strive to provide people with supports that are in line with their expectations and preferences, and will support them to live their best life.
Providers are required to ensure that while implementing consumer choice and working with diversity, risks are identified and managed to ensure targets and outcomes are met, outcomes which require services to be what the consumer wants but are also safe and based on best practice.
Teams must juggle these requirements while working with consumers of increasing age, frailty, comorbidities and polypharmacy, and this along with changes in aged care regulations and reforms and the shortage of aged care workers, can create the perfect storm (risk) for something to go wrong.
The diversity of risks that providers must manage requires all the workforce to think of how the small things may create larger problems. Consider also the diversity in these risk findings against organisations which led to a finding of unmet:
■ an absence of documentation of consumer needs and preferences and clinical or other strategies/interventions to support consumers nearing the end of life
■ Care and Service Plans not reflective of complex care required or timeliness of reviews and suitable workforce to review
■ deterioration in consumer care with no timely referrals made
■ incident forms not always recorded consistently, or incident forms were identified in progress notes, but not updated in Care and Service Plans
■ lack of workforce knowledge regarding high-impact highprevalence and no clinical risk assessments in place
■ inappropriate locking of doors and bed rails in place, where the workforce lack knowledge regarding restrictive practices
■ assessment noted an unresolved wound, but no strategies were undertaken to consult or refer to wound care practice experts.
Clinical governance is critical in aged care settings. To make sure your organisation is on track, the following checklist is a useful guide.
Ensure you have a strong clinical governance commitment from the board to the floor.
Ensure you have a comprehensive clinical governance policy that addresses the key areas of care and your team know the policy.
Audit and review your clinical governance systems. Implement a comprehensive education and competency assessment program regarding clinical care.
Ensure registered nurses (including contracted RNs) have a good understanding of clinical care and what is required, how to escalate concerns and ensure contract education records are available.
Imbed regular auditing of consumer files into your monthly reporting processes.
Update your workforce training in risk assessment and high-impact high-prevalence clinical care management.
Support your teams with access to clinical experts and best practice guidelines.
Assess the knowledge and skills in areas of clinical governance for your team.
Create an environment where the team know it’s ok to ask questions and ask for support or more training.
Fleur
Hannen, Managing Director, Critical Success Solutionswww.criticalsuccesssolutions.com.au
Working
Our team includes industry experts who are focused on helping your facility to meet aged care quality standards. Working side by side, our hands on approach can assist you to build capacity in your team, set the benchmark for outstanding care in your organisation or manage your day-to-day when you need a helping hand.
In response to the introduction of the existing standards, CSS developed our successful Aged Care In a Box solution: a system of policy and procedures, providing plain English policies full of innovation, best practice and guidance for you to support care and service delivery in your residential facility or home care service.
Our user-friendly documents incorporate diagrams and flowcharts to provide meaningful, easy to follow content and can be implemented by our team as part of the comprehensive training our consultants offer providers.
Talk to us about how Aged Care in a Box will evolve to meet the requirements of the new Standards and the new support at home program.
CSS has partnered with many providers in our industry to offer comprehensive education to all levels of workforce on the requirements of our industry.
Our experience tells us that one size does not fit all, from standards education, new graduate programmes to mentoring managers and executive. Talk to CSS about a program that meets your needs.
CALL US TODAY! Phone 02 9052 0292, email us on info@cssconsulting.com.au or visit criticalsuccesssolutions.com.au
With 20 years in the industry, Critical Success Solutions (CSS) can assist to improve your governance, compliance, frameworks, sustainability and adaptability
your partner in compliance.
Our team at CSS includes industry experts who are focused on helping your facility to meet aged care quality standards.
side by side, our hands on approach can assist you to build capacity in your team, set the benchmark for outstanding care in your organisation or manageyour day-to-day when you need a helping hand.
Oscar Wilde once said, “There is only one thing worse than being talked about and that is not being talked about.” He might have added, in the case of aged care residents talking about maintenance.
Delighted residents are only too keen to discuss the amenities of a facility. Maintenance on the other hand, is a topic reserved for more challenging conversations. Common complaints include the length of time it takes to carry out a repair, quality of workmanship, and the timing of upkeep such as repainting, recarpeting or refurbishments.
While maintenance is a key area of responsibility of aged care facility operators, it is rarely an area of expertise for them. Residents often have strong views on the quality of maintenance that they observe, frequently drawing upon their own expertise, or that of a relative or friend in reaching their conclusions.
It is hard not to sympathise with residents’ criticism of maintenance in the aged care environment, it is their home after all, and it would frustrate most people to see work done that they cannot control, and to which they feel they could add value.
To avoid these issues arising, clear and effective communication is key. From telling residents how long it will take to respond to or resolve a maintenance issue, to letting them know who is doing the job, a good degree of transparency helps ease worried minds.
Forward works programs are of value to help plan for the replacement or refurbishment of assets in the long term, say ten years. This might include repainting, recarpeting or roof replacement works. These programs help operators to match scarce funds with greatest business need.
Regular asset audits should be carried out at least every three years, with the findings used to update the forward works programs. This means your plan remains current and helps ensure that funding is available for works as and when required.
In some other sectors, to help meet the challenge of asset maintenance, outsourcing has been popular. While few aged care facilities are large enough to support an outsourced contract, by bundling sites that are geographically close together into a single contract (even if run by different organisations), outsourcing can present a practical solution. It can also be advantageous for organisations with multiple sites.
A robust, transparent approach is key to taking residents on a journey towards effective asset maintenance. And whether an outsourced solution is selected, or a provider decides to organically develop their asset maintenance capabilities inhouse, there are key mechanisms that can be put in place to ensure that a best-practice approach is being implemented.

For example ISO 55000, is the global standard for asset maintenance and while a fully accredited solution may not be appropriate, aligning asset maintenance with this methodology helps ensure and demonstrate to all stakeholders that a best-practice approach is being employed.
The COVID-19 experience has reinforced that we live in volatile times, where the status quo cannot be taken for granted and the more that we adopt consistent, standardised, robust approaches to day-to-day activities including maintenance, the stronger and more resilient the model will be when it is exposed to unexpected stressors.
Donald Macdonald, Director, Macdonald Lucas www.macdonaldlucas.com











Demand for retirement living is set to grow, according to a new study by Catalyst Research in partnership with Council on the Ageing (COTA).
When asked about future accommodation needs, the survey found that four in ten Australians over 60 would consider retirement living. Further, 8 per cent prioritise retirement living ahead of other options including staying at home or downsizing. This compares favourably with the 6 per cent currently living in a village or land lease community.
Giving older people a sense of safety and security while still maintaining complete independence as they age is part of the attraction of retirement villages. However, the industry is hampered by reputational issues, and a big one lies in the complexity of contracts.
The Catalyst Report - RL gathered feedback from over 6,500 Australians including residents, shoppers and ‘rejectors’, to delve deeper into the reasons why people consider or dismiss retirement living. The study looked at triggers, motivations, information sources, evaluation criteria and barriers.
It was clear from the study, that one of the things holding the industry back is confusion around and mistrust of contracts. Almost four in ten ‘shoppers’ see contract complexity as problematic. Current residents experiencing this will tell others and the bad news will spread.
Here are some of the comments in relation to contacts, that were extracted from the study:
■ “It’s a one-sided contract.”
■ “The contract is It is too complex for all advisers including COTA, Consumer Affairs Victoria and the Residents of Retirement Villages Victoria (RRVV)”
■ “Unconsciousible contracts, fraud, legislation ignored, deceitful marketing.”
■ “We didn’t see our contract until almost two years after we moved in. There was no discussion on putting things back to standard. We were told we would have new carpets and inside painting every seven years. Lies and more lies.”
The complexity of contracts contributes to the high level of disputes. One in four residents have been directly involved

in a dispute and a similar number is aware of a dispute within their village. That’s an awful lot of disputes, and fewer than four in ten are enthusiastic about the dispute experience. According to the study, only one in three residents sought legal advice before committing to their purchase.
Some of the comments around disputes included:
■ “I have been subjected to bullying and intimidation and have applied to SACAT for a hearing.”
■ “Despite having a very committed and active Residents’ Committee, it is very difficult to get a good outcome when disputes arise.”
■ “The village manager practises retribution to those who raise issues she disagrees with or controls. They do not manage disputes according to the code of practice.”
Findings from The Catalyst Report - RL raise questions about the need for the industry to work collaboratively to simplify and standardise contracts, understanding that this is complicated by the fact that retirement living is regulated separately by each state or territory.
In 2013, the NSW Government simplified contracts making them easier to understand, and while that’s a step in the right direction, it was a long time ago, and there’s a lot more to do.
Elizabeth Teece, Policy & Member Support Officer at Aged Care & Community Providers Association (ACCPA) says the introduction of a compulsory standard retirement village contract by the NSW Government has made contracts more readily understood and useable, and other jurisdictions in Australia could benefit from a similar approach.
“As a priority, we need to ensure prospective village residents are provided with transparent and easy-to-understand contracts and encourage them to seek independent legal advice,” says Elizabeth.
“The work that ACCPA is doing in partnership with The Property Council and Residents’ Associations to move towards plain English contracts Australia-wide will be of great benefit to the industry.”
It certainly is a welcome move, and none too soon.
Kevin McCreton, Founder, Catalyst Research www.thecatalystreport.com.au
Four in ten Australians considering retirement living, but contracts pose a barrier
Australia is currently in the midst of the biggest intergenerational wealth transfer in history, with Baby Boomers set to hand over $3.5 trillion to the next generation.
However, new research shows that over 40 per cent of Australians are yet to have important and proactive conversations with their loved ones about inheritance, despite 74 per cent saying these conversations are necessary.
In fact, the research shows that 20 per cent are not even sure how to begin the discussion with their loved ones despite almost half believing that having the conversation about a legacy before a person passes away will cause less conflict among beneficiaries.
The research, commissioned by financial educator and communicator Vanessa Stoykov, reveals the compelling need for Australians to be confident and comfortable having conversations about money.
“It can be tricky to navigate difficult conversations around money and inheritance but talking openly to loved ones is a legacy and gift in itself,” said Vanessa.
“I am certain aged and community care providers would understand the challenges given they often need to traverse sensitive topics with residents and their families.
“Providers may be able to assist residents and their families by running programs to help them start these conversations or provide meeting facilities to enable people to gather together.”
As to who should start conversations about inheritance, Vanessa noted this will depend on each situation.
“The biggest thing for people to remember in this process, is that you need to do it well before it is too late,” said Vanessa.
“I encourage both parents and their children to plan for and set these important conversations in motion.
“What’s important is that older people give proper consideration to what they want to leave behind for their children or other loved ones.”
In the new book The Five Conversations About Money That Will Radically Change Your Life, Vanessa provides four tips for people starting conversations about inheritance.

1. Prepare. Really think about your own relationship with money and your legacy. Be clear on what you think before you say anything.
2. Meet. Call a family meeting for a date at least a month out, preferably with everyone in the room, or with everyone present via video so nobody is left out.
3. Be clear. Set an agenda and give it to everyone. What are the key areas you wish to talk about? If you want to really own the conversation you need to outline what you intend to cover, and ask for comments along the way so you make sure you’re being heard.
4. Be available. Be prepared to set other meetings. Do not expect one meeting to fix it all. Money conversations and strategic decisions do not happen quickly. Be prepared to follow up and set another meeting in three months to give everyone time to fully absorb and think about what you have shared.
While it can be difficult to find a way through complex family relationships, having these conversations can do wonders to bring people closer.
“I think providers would potentially see parallels between these types of conversations between families and broader conversations about health decisions and know from direct experience the importance of clarity for all concerned,” said Vanessa.
“The process can be a real gift in bringing families together, or at the very least, making clear a direction for all to follow, avoiding arguments over grey areas in the future.”
Vanessa Stoykov, Wealth Educator and Author www.vanessastoykov.com.au
This year’s innovAGEING National Awards have just been announced, demonstrating how far Australia’s aged services industry has come in terms of its ability to respond to changing needs and consumer demands, through innovative products and practices.
Across the six awards categories, there have been outstanding examples of innovation, with the ultimate aim to provide a better ageing experience for older Australians who require aged care services.
“Innovation in aged care is not just about having the right technology and set up, it’s about supporting the workforce to deliver better care, and equipping them with the right tools and systems,” said Merlin Kong, Head of innovAGEING –Australia’s innovation network for age services.

“I’d like to congratulate all the winners – as well as the finalists –not just for being recognised in our awards program, but also for their commitment to supporting better aged care in Australia.”
The awards were made possible through the ongoing support of innovAGEING Foundation Partners the Commonwealth Bank and KPMG Australia
innovAGEING also wishes to thank the awards judges:
■ Belinda Hegarty, National Head of Strategy and Insights - CommBank Health


■ Laura Haylen, Associate Director, KPMG Australia
■ Ian Poalses, QLD State Manager, Aged & Community Care Providers Association.
Aidan O’Flaherty and his team recognised an issue in the industry with asset management from an aged care and retirement perspective. Aidan moved to create Asset Management Software to specifically service aged care and retirement living providers.
Building Asset Journey within six months, Tulich started to sell the product to their peers, resulting in 28 clients in less than nine months. The key point of difference was that the vision of Asset Journey was from an operator’s perspective.
Aidan is looking to continue to grow Asset Journey, to help aged care and retirement villages manage their assets more appropriately.
Stephen Milsted, Manager Hospitality Services, noticed that although the gardening team had set up herb gardens around Lifeview homes, along with some raised planter boxes, as part of the resident gardening program, there wasn’t a lot going on.
After consultation with the gardeners, chefs and residents, the Planting with a Purpose program was born. The program now sees residents successfully teaming with chefs and gardeners to cultivate and grow fresh produce for Lifeview’s kitchens.
Each quarter, when planning the season’s menus, which is done in consultation with the residents, the chefs advise the gardening team of the fresh produce they will be requiring. Residents are involved in everything from germinating seedlings, to planting, tending and harvesting the produce.
Atticus Health imagined a new concept of ageing where an older person is supported to live at home by a truly integrated team, working in unison in an efficient and viable manner. Through the Atticus Healthcare Network, they have built a model of well integrated health and home care.
Using technology where appropriate for the free flow of information, less duplication and greater continuity of care, the Atticus model allows a house-bound person to continue their relationship with their regular GP.
For example, particularly with the management of complex wounds, their Registered Nurses consult with their Geriatrician for advice, leading to better decision making and improved clinical outcomes. They can also involve medical specialists (often via Telehealth), when needed.
Inclusee’s Development Team was tasked with creating a social program to connect senior participants with volunteers in disparate geographic locations, for social support in group
settings, utilising digital technology, which became known as Interests2Enjoy. However, they soon realised that lack of skills was a barrier.
They recognised that rather than teaching seniors to use the technology, they needed to come up with a technology solution that didn’t require teaching.
Inclusee’s solution was a Samsung tablet, preloaded with a SIM card that provides 10 gig per month of data. It is a loan tablet that is totally free for the senior participant. The device is paired back to ensure ease of access, including slowing down the reaction time to accommodate dexterity issues, enlarged fonts, an app to verbally read out the text on screen, and a clean simplified interface.
Inclusee was then able to offer various programs to connect participants, to provide valuable social support to people in their own homes.
McKenzie Aged Care Group observed their mandatory training program was similar to other providers and that many staff were unnecessarily repeating training. An analysis estimated that this was costing the sector 8.02 million dollars per annum.
McKenzie recognised an opportunity to align staff, processes, data and technology to reduce the burden of repeat training and refocus that energy towards high-impact training to improve care.

To achieve this, McKenzie and Ausmed created an ‘Aged Care Industry Passport’, leveraging Ausmed’s learning platform. This resulted in the Ausmed Passport™, a digital certificate that people working in aged care can carry with them from one employer to the next to evidence they have completed mandatory training relevant to and recognised by the sector.
Anticipating the changes required to transition from the ACFI Pain Management model to the new AN-ACC requirements, Whiddon’s Strategy & Innovation Team developed, tested and scaled new evidence-based methods of pain management and reablement programs for residents.
With expert input from University of Sydney’s Clinician Researcher, Dr Jennie Hewitt, they ran a three-month pilot of Whiddon’s Exercise4Life Program. Customisable to residents’ needs, it involved each resident receiving their own tailored program, delivered either one-to-one or in a group setting.
The trial proved very successful, with a 50 per cent reduction in overall pain symptoms, 20 per cent improvement in overall mood and happiness, and improvement in physical function for participants at the end of the program.
Linda Baraciolli, Aged Care Today Editor & Communications Advisor, Aged & Community Care Providers Association www.innovageing.org.au
In October, Dementia Australia launched the free mobile app, BrainTrack, for people to privately monitor and better understand suspected changes in their cognition over time. The app enables individuals who may have concerns about changes to their cognition to track these through a series of games. A report of their results can be produced and shared with their GP or healthcare professional as a conversation starter to support an earlier dementia diagnosis.
Dementia can impact anyone at any age, including people in their 30s, 40s and 50s. BrainTrack can be used by anyone –at any age, including individuals who simply want to know more about brain health and healthy ageing.
BrainTrack incorporates fun, travel-themed games adapted from validated cognitive testing, where users are prompted to log in each month to play the games and monitor their results. Games focus on specific cognitive domains covering executive function, visuospatial function, language, visual recognition and memory.
There are specific resources for GPs and healthcare professionals, including interpreting a patient’s results, what the results might mean, and tests that can be used to validate them. There is also information including modifiable risk factors and guidance on having a conversation with a patient.
While not intended to replace a formal cognitive assessment, BrainTrack supports the early identification of cognitive changes over time that may warrant further testing. Having a conversation with their GP early when a person has concerns about changes to their cognition may lead to earlier diagnosis.
Currently a diagnosis of dementia takes an average of three years. With up to half a million Australians living with dementia – projected to increase to 1.1 million people by 2058 –improving early diagnosis must be a priority.
Like other diseases we know that the earlier the diagnosis, the better the outcomes. An early diagnosis of dementia empowers and enables people living with dementia, their
families and carers to better understand dementia and to manage their diagnosis on their terms. It provides the opportunity to access the right support at the right time, which can enable people to maintain their independence and functional capacity for as long as possible.
Health and allied health professionals play an essential role in helping people living with dementia to live well for longer. By assessing physical and cognitive issues they can provide interventions to support the maintenance of current strengths and capacities, improve skill acquisition and promote recovery, enablement and rehabilitation.
Through Dementia Australia, healthcare professionals can receive education on how to empower patients impacted by dementia to access appropriate services, information and supports. With patient consent, Dementia Australia can contact the patient with suggestions of appropriate support. Research indicates that the use of allied health services can slow the progression of cognitive and functional decline, improve quality of life and delay or prevent residential aged care admission.
The more healthcare professionals know and understand about dementia, and how Dementia Australia’s support and services can support their patient, the better the system and healthcare experience will be for all.
I urge all healthcare professionals to learn more about dementia and equip themselves with BrainTrack as a key tool designed specifically to support individuals and their GPs to start a conversation to support an earlier dementia diagnosis.
Together, we can help people living with dementia to access essential services and supports, and live well for longer.
BrainTrack was funded by the Australian Government. It is free to download and is available through the Apple App Store and Google Play. For information on how to best support patients, call the National Dementia Helpline on 1800 100 500.
Maree McCabe AM, CEO, Dementia Australia www.dementia.org.au/braintrack

When I first met Bobby Redman, on one of those video conferencing services we all use since COVID-19, her robot companion dog was yapping in the background and at one point she muted our call to respond to a prompt from her home digital assistant.
Communication, companionship, warnings, sequencing; Bobby has surrounded herself with AI technology, but it’s no hobby or indulgence.
“I have my own carer, I am my own carer, technology is my carer,” Bobby told us at the International Dementia Conference 2022: Brave New World, where she was a speaker.
Bobby is a retired psychologist and a dementia advocate who remains safely at home six years after her frontotemporal dementia diagnosis and two years since she was warned to prepare for life in residential care.
Now 73, Bobby manages a condition that causes frequent memory lapses and puts her at risk of falls, by deploying technology devices including the Google Assistant movement sensors throughout her house and voice reminders she has recorded onto her mobile phone.
The sensors not only detect if Bobby falls, they constantly feed information to a phone app that analyses her movements, to help her become aware of deviations from the norm.
“I recognised as a psychologist that changes in patterns of behaviour are the first indication that things are going pearshaped,” she said.
When she journeys from home, which as an advocate and researcher she does frequently, Bobby wears a personal alarm pendant that also tracks her movements by GPS.
Two years ago, Bobby was told by an assessor that she was increasingly at risk in her home – particularly from falling and from accidents due to memory lapse, like burning her food –and should prepare to be living in care within 12 months.
“I said, ‘you’re kidding, I’m not ready for residential care’. I’m out in the community, I’m an advocate, I work.”
Through her own research and with help from technologist friends at The University of Sydney and The University of Queensland, Bobby found solutions to her everyday challenges.
When I visited her home, I counted six different technologies working for her. I feel like a Luddite when I’m around Bobby, and at the conference we saw many people scribbling notes on her technologies and techniques.
Using smart sensors, smartphone apps and digital assistance is extending by years the time Bobby stays independent and in her own home, which is where most of us are happiest and most productive.
Bobby believes her robot companion dog will be of increasing value in reducing her stress and anxiety while she remains at home.
During the conference, we heard from Tom Stephens, whose Californian company Tombot will soon bring to market a robotic, interactive emotional support animal, claimed to be the most advanced, realistic example of these devices.
‘Jennie’ works both as a companion for people living with dementia and a platform for monitoring their safety and health, collecting data for care-givers and medical providers.
The foundational idea for developing the robot came when Tom was forced to take away his mother’s pet dog because, having developed Alzheimer’s Dementia, Nancy could no longer care for it safely.
As Nancy’s loneliness and depression were exacerbated by the loss, Tom began the work that gave rise to Jennie and his understanding of emotional attachment to robotic companions.
“We realised this was not an entertainment device, this was something that seniors chose to care for,” said Tom.
“This idea of emotional attachment became key to our product design, and (for people) to attach to it, it couldn’t just be a token device.”
Jennie was designed, with the assistance of animator Jim Henson’s Creature Shop studio, to look and behave as a Labrador puppy, triggering the owner’s instinct to care and promoting the emotional bond that generates health and wellbeing benefits.
Suffice to say, we are seeing technology help defy the odds for people living with dementia, and the applications for robotics in supporting people with dementia and other medical conditions will continue to expand into the future.
John Sutherland, Chief Information Officer, HammondCare www.hammondcare.com.au

















In response to the Aged Care Royal Commission report, the Federal Government identified five pillars of reform and allocated commensurate funding for their implementation, two of which should be in the forefront of planning for aged care providers: daily average care minutes for each resident increased to 200 minutes per day, including 40 minutes of registered nurse time; and a Registered Nurse on site for a minimum of 16 hours per day.
These are highly commendable reforms that will improve the quality of care for 240,000 people using residential care and 67,000 people using residential respite care each year, delivering levels of care that were never previously available in most residential aged care homes. But it does mean a lot of work for aged care providers ahead of the changes.
Given that these minimum care times become mandatory in 2023, residential aged care providers will need to implement systems that can accurately track and document carer and resident interactions, with the capacity to provide auditable records.
Fortunately, technology exists in the shape of Real Time Location Services (RTLS) that, in conjunction with Bluetooth Low Energy (BLE), can eliminate tedious and potentially inaccurate staff generated paper trails and deliver quantifiable data electronically.

RTLS is not a new concept, it has been used extensively, in varying forms, within the transportation and logistics industries for many years. However, its use in aged and health care is a relatively recent innovation, coming about only after the development of IP based nurse call solutions. That said, residential care operators have quickly recognised RTLS’ inherent value with significant interest and adoption. Every IP based nurse call point with an integrated BLE beacon provides specific detail of where residents and staff are located. When a carer responds to a resident’s initiated assistance call, or a RN comes within range of the
BLE beacon during their scheduled attendance, their mobile device immediately ‘pairs’ with the beacon, date and time stamping the duration of contact.
RTLS is a software configured system, so it is essentially future proof with the ability to add enhanced functionality with ongoing ‘over the air’ (OTA) software updates as required.
As the security of accumulated data is paramount with any IP based solution, the adoption of a highly resilient cyber security controls such as Zero Trust Architecture (ZTA) must be employed to minimise the risk of malicious cyberattacks.
RTLS via low energy Bluetooth technology not only provides facility management with alert activation, it also accurately details, staff response time, location and actual time in attendance.
Residents and their families derive greater comfort knowing that the minimum face-to-face care is being consistently delivered, and facility operators can feel confident that the carer-to-resident standards are being automatically recorded for regulatory compliance.
RTLS applications present many benefits to the aged care sector, from operational efficiencies through to enhancing staff safety and resident care. In addition to supporting personal safety, RTLS can also help track the whereabouts of tagged equipment, contributing to productivity and resource savings.
Vital support functions such as scheduled room cleaning can also
be monitored right across the BLE beacon’s coverage area. Such end-toend accountability of all carer activity not only provides an auditable record, it also gives facility management an invaluable insight into time management, inter-site benchmarking and staff productivity, enabling the most effective allocation of precious human resources across rotating shifts.
As the aged care sector transitions to the ‘five key pillars’ of aged care reform, applied technology and innovation like RTLS and BLE will undoubtedly become a major contributor to the delivery of these critical initiatives.
Sean Griffin, Marketing Consultant, Alexys www.alexys.com.au
How digital technology under the new AN-ACC model ensures a more accurate and nationally consistent assessment process
Following the latest changes introduced by the Australian Government regarding the continued development of the Australian National Aged Care Classification (AN-ACC), there are an array of imminent technological benefits to support better care.
In response to the Aged Care Royal Commission, the government has introduced mandatory care minute standards for residential aged care. The initial care minute requirements have been set at an average of 200 minutes per resident per day, including a minimum of 40 minutes of direct care from a registered nurse, with registered nurses rostered for 16 hours per day.
On top of this, the government has mandated a change in the system following a series of recent studies – one of which analysed surveys submitted by 50 per cent of aged care homes across Australia. The study revealed that the average care time delivered is 175.8 minutes, and 84 per cent of aged care facilities are delivering less than the required 200 minutes of care per resident per day.
With results demonstrating that most aged care homes may not meet new mandatory minimum staffing standards, it is vital that aged care providers implement the right solutions to ensure that all care is evidenced efficiently and accurately.
Subsequently, aged care homes should consider running reports using digitised software to calculate how much care is being provided – enabling sufficient time to adjust staffing levels if necessary.
A recurring theme within the aged care sector, especially residential care, has been the inadequacy of funding available to provide safe and quality care. Using technological advancements to their full potential can make the dollar go further.
For example, using data from statistical analysis and benchmarking can provide insights into operations that are not immediately obvious, and appropriate responses can be made. Additionally, data enables aged care providers to tailor services to meet the needs of each person in their care.
We now live in a world where technology is integrated into everything around us and the right technology can enhance the mental and physical wellbeing of others. Providers are digitising their care environments because they understand that care technology is the key to supporting the caregiver at a rate never seen before, and those that don’t take this step risk being left behind.


Through implementation and application of the right technology, staff can evidence their care accurately in real time.
The information is saved instantaneously within a secure online portal accessible to all those in the organisation who have access, and carers can save time, reduce workloads, minimise errors and, most importantly, focus the majority of their time connecting with residents and providing meaningful support. Ultimately, the funding model is moving from a task-driven model to a more person-centred approach, which will mean aged care homes will need to continue evidencing care to secure the necessary funding. On top of this, further utilisation of technology will ensure the assessment process will be more accurate and nationally consistent. At the same time, the burden of paperwork will be removed altogether, allowing carers to spend more time providing safe, effective and person-centred care.
Overall, the mandated changes continue to showcase the agile capabilities of technology that are empowering all areas of aged care operations. With all these beneficial changes, we can rest assured that technology is the key to continuing the delivery of outstanding care throughout Australian aged care homes.
Person Centred Software stands ready to support the aged services industry with our app-based Clinical Care System, which allows aged care home staff to digitally plan, record and monitor the care of residents in real time. Used by over 150 aged care homes, the software has been developed with over 20 years of experience in aged care, and is improving the lives of residents and care staff.
Tammy Sherwood, CEO, Person Centred Software Australia & New Zealand www.personcentredsoftware.com.au
Cyber security is often overlooked, but it shouldn’t be
Recent cyberattacks targeting large corporate organisations have once again raised awareness that we are in an environment that in a large part goes unseen and is not often understood. It is not until the ‘proverbial hits the fan’ as it has of late, that attention is once again focused on the issue.
The cyber environment impacts all of us in significant ways, from our daily phone traffic, emails, texts, tweets, and even more damaging things like our bank accounts, Medicare and identity document details, which are tracked and stored in hundreds, if not thousands, of places.
I recall not so long ago, how the general community was in uproar over the idea that, at the time, the Australian Government wanted to introduce an ‘Australia Card’. No, never, we said, it would be a total breach of our privacy and rights. We would have nothing to do with it. That was in 1985.
How naive we were, all they wanted to store was basic information, most of which they already held in a dozen different departments.
Instead, by default, we opted for total and unmitigated disclosure of every aspect of our lives and then some, in any portal we can find, from online games to banking to travel and online purchases.
You can barely breathe these days without putting personal data into a myriad of applications and websites. The process invades our past, our present and our future, as well as everyone in our chain of contacts.
The management team at e-Tools Software decided over a year ago that there was a need to afford the appropriate protection for aged care and disability providers, a vast number of whom use e-Tools applications and services.
e-Tools Software embarked on an ISO 27001:2013 Information Security Management System accreditation journey. The process took approximately 12 months and considerable financial commitment, but we got there.
e-Tools Software is now certified. We demonstrate international-standard controls for data protection, to assure the integrity of our clients’ data. This is essential to provide the level of data security that the industry needs and is entitled to expect.
ISO certification is issued only to highly efficient organisations that prove they have a management system of an internationally certifiable standard and have a commitment to continuous improvement.
This protects our clients’ data and enhances our systems to allow e-Tools to further expand its security protections going forward.
Our commitment is an example of ‘walking the talk’. As a passionate industry leader, e-Tools is proud of this achievement, but the sole purpose is to provide our clients with the comfort that we are taking every step to ensure the best data security possible.
There are many steps that providers of aged community and disability services can undertake to further enhance data security, but any actions should include partnering with providers who themselves take data security seriously.

Together we can go a long way to combat this scourge, which frankly is data terrorism. These privacy breaches are destructive, dishonest and breed mistrust.
e-Tools will be communicating with its clients on a range of areas in which they can improve their data protection internally, as we do our best to provide the highest level of ongoing data security. Make sure your data protection partner is at the top of the game, too.
David Powis, Managing Director, e-Tools Software www.e-tools.com.au
Launched in April 2021, the Serious Incident Response Scheme (SIRS) is an initiative that helps prevent and reduce incidents of abuse and neglect in residential aged care services subsidised by the Australian Government. Since 1 December 2022, the scheme will be extended to include home aged care and flexible care delivered in a home or community setting.
Incidents are split into two categories and require different reporting obligations:
■ Priority 1 must be reported to the Aged Care Royal Commission or police within 24 hours of becoming aware of it occurring.
■ Priority 2 must be reported to the Aged Care Royal Commission within 30 days of becoming aware of it occurring.
With timelines playing such a critical role in responding to serious incidents, finding a standardised method to lodge incidents from anywhere is now essential, and for many providers, these systems are not yet in place.
Although reporting obligations have now expanded, those responsible for remaining compliant have not changed; the pressure is still on carers to ensure incidents are reported correctly.
“Even though there is a dedicated team to handle compliance requirements surrounding incident data, the responsibility of accurately reporting an incident ultimately falls on carers,” explains Bremmar’s Lead Aged Care consultant, Rushad Billimoria.
“Having the right reporting technologies in aged care can ease this added pressure, automatically complying with government regulations and making life a lot easier for all involved.”
Ultimately, new technology creates efficiency in the incident reporting process. It’s there to make life easier for carers and other executives, giving peace of mind that people can confidently focus on their primary job – to care and assist –without having to worry about extra administration.
Without a viable, long-term mobile reporting system, this could see travelling carers not only under more pressure to recall important information well after the fact, but also falling foul of updated regulations.
With so many vendors and technological choices, which is the right one to help aged care providers remain compliant?
Apps like Bremmar’s Incident Management App can be a game-changer in incident reporting processes.
As specialists in the aged care sector, Bremmar has had years road-testing the best technologies for the industry. In our opinion, it’s hard to go past Microsoft Power Apps.
This tool is part of the Microsoft ecosystem, making it easy to access and connect information within the Microsoft 365 platform as well as with third-party applications.
Built in response to industry needs, the Bremmar Incident Management App consolidates the reporting process into one system, enabling organisations to connect incident data sources, create custom digital forms, and implement effective business process automation. Organisations are then able to:
■ streamline incident reporting processes
■ automate notifications and implement efficient approval processes
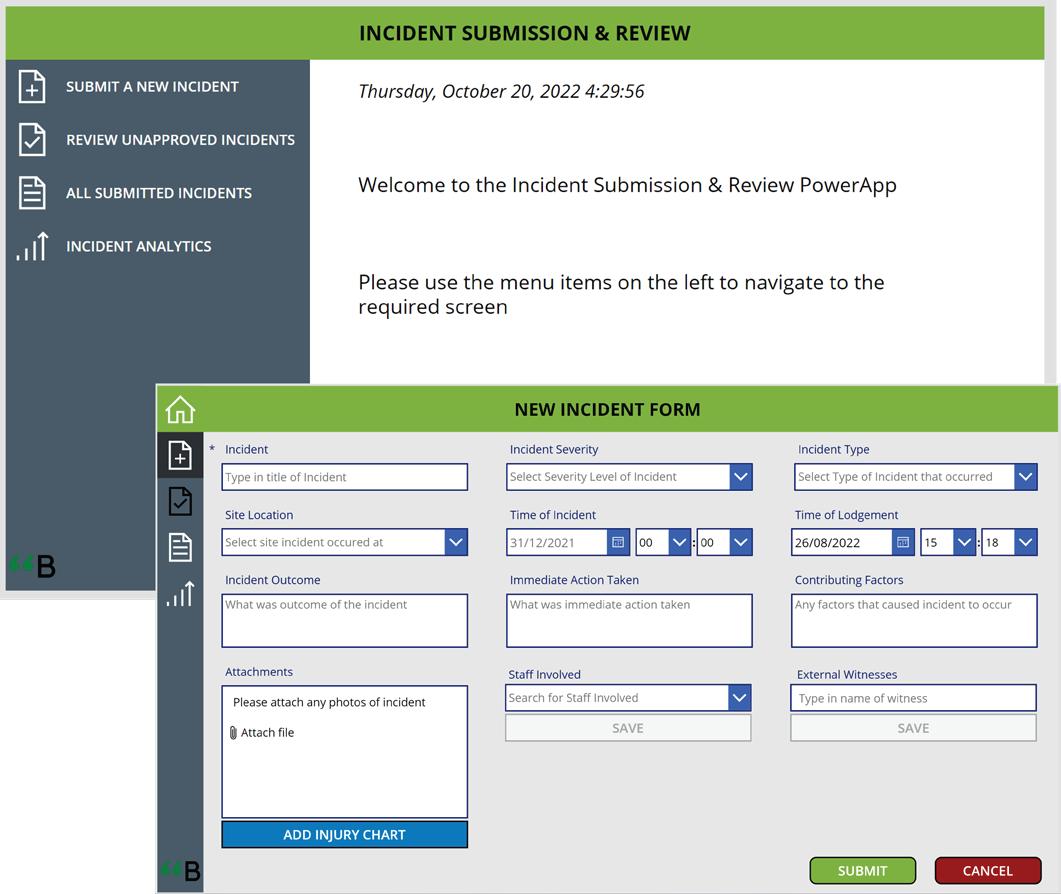
■ set dynamic dashboards to have visibility into vital data points
■ build a bespoke incident reporting solution to cater for your specific needs
■ develop a custom Incident Management app with Bremmar.
Although developing an improved digital workflow automation for incident reporting may seem complex and intimidating, the importance of getting it right means organisations need to take the time to make the switch. Bremmar can assist with a no cost Power Apps planning, scoping and consultation session to suit your specific requirements.
Rushad Billimoria, Aged Care Consultant, Bremmar www.bremmar.com.au/agedcare-incident/
Why manual or paper-based processes are no longer acceptable
Support for mental health should be at the top of the agenda for the aged care sector for care workers, care agencies, service users and all stakeholders in the ‘circle of care’ in 2023.
However, it can be approached from different angles, including the adoption of new systems and processes that lighten the burden of work for the care agency and carer, and improve communication with clients and loved ones.
For example, supporting service users with mental health care requirements means that agencies need to provide solutions that may go beyond the remit of one’s official care package, such as lengthy call times and in-person sessions. However, the full-on nature of the work and constant support required can take a toll, both mental and financial, on the carers.
In this case, adopting tools that can help manage the tasks involved and ease the workload can be of benefit to both carers and clients. Something as simple as noting which carers are preferred by a client and finding the right match between the two parties is a key factor in supporting mental health and wellbeing.
Despite this kind of work having a strain on carers, with many not being paid for the additional demands, they still want to provide the best care they can. Because of this, it’s important to support carers to help make their lives easier and more efficient.
Another way to look at this issue is to consider the shortage of staff in the care industry that Australia is facing at the moment. According to an industry report, the country will need more than 200,000 full-time carers by 2050. As we have seen in other countries, what this shortage means is more pressure not only on carers, but also on patients’
CareLineLive conducted a recent survey, in which 40 per cent of carers in home care cited the inability to properly care for clients (together with stress) as one of the key reasons for wanting to leave the profession.

From home care workers’ point of view, it is important that they have access to tools that can make their job easier and help them focus on clients’ care. It may not mean much for those not involved, but not having to spend a lot of time writing reports can make a big difference to people on the ground.
For example, being able to provide their notes using a speech-to-text feature can help relieve anxiety and reduce the workload. It can help them spend more time delivering care and feel more connected to their clients and, therefore, be happier in their jobs and less likely to leave.
Providing access to family members and friends with all the information about the care their loved one is receiving can give them peace of mind and, just
as important for the agency, can mean fewer calls into the office or other administration.
An outcome of the pandemic is that more older people are using technology to communicate with friends and family, with 77 per cent of over 65s reported to use the Internet at home in 2020, while the number of those aged 75 or older using the Internet has nearly doubled in the seven years leading to 2021.
There is no doubt that digital transformation is playing a vital role in the provision of services for older people across the world, as well as helping carers be more efficient with their care delivery. This translates into better mental wellbeing for all.
Ultimately, we need to encourage greater conversations and support for the mental health of both staff and clients. CareLineLive stands ready to support the sector with our awardwinning all-in-one cloud-based home care management software platform, and to continue to innovate, to support the care industry.
Josh Hough, MD, CareLineLive www.carelinelive.com

Staffing shortages, limited time and resources and increased compliance requirements –the age care industry is under increasing pressure to do more with less.
Thankfully, modern technology can address a lot of these pain points. There are some great examples of aged care facilities in Australia that have embarked on a digital transformation path are automating manual processes and increasing staff efficiency.
For staff, a lesser focus on administrative tasks ensures they can focus on what they do best – providing better care. For aged care providers, it means doing more without having to hire additional staff. And for residents, it ultimately means better experience.
But working with aged care facilities every day, I am very aware that such digital transformation often includes large-scale changes that many providers simply can’t afford or facilitate all at once. So here are a few things to consider before embarking on such a project.
In a sector impacted by ongoing funding, policy and technology disruption, it is essential for aged care providers to have core systems that are flexible, scalable and future proof.
An investment in digital technology is an opportunity to future proof the organisation to ensure it and adapt to future challenges – be it growth, or policy and legislative changes.
Experts agree recent high-profile cybersecurity attacks are only the tip of the iceberg. Aged care providers
are privileged to be entrusted with incredibly sensitive data about residents and staff, but such privilege comes with a responsibility to invest heavily in security.
Knowing that data security is taken care of by a trusted partner means providers can focus their time and resources on their core business.
At TechnologyOne our global One ERP solution delivers the highest level of security and privacy to ensure our customers are protected by our multitiered security measures and accredited procedures.
With such a large-scale transformation projects, finding a technology solution that can be implemented in stages can be an ideal compromise, moving each facility in the right direction, at their own pace.
A step-by-step solution might be helpful, where aged care providers can take up increasing levels of automation over time, while SaaS will allow work to be done anywhere, at any time and on any device.
For example, our TechnologyOne OneCare solution fully integrates with existing ERP systems. This means aged care providers don’t have to undergo their digital transformation in one giant sweep. Instead, they can transition to OneCare in stages without any disruption to their existing systems and operations.
The aged care industry and its regulatory environment are unique, and facilities need a partner and solution that addresses key challenges across
the aged care sector. Having been providing software solutions in Australia and New Zealand for over 35 years, our OneCare solution has adapted both in technology and functionality to handle the most complex of situations.
Our deep industry expertise means OneCare integrates seamlessly with patients, residents, or client management system, streamlining business processes, and allowing providers to focus on better health outcomes. Our broad enterprise footprint consolidates multiple core systems into one code base and a single source of truth, spanning financial and supply chain management, resident and client billing.
OneCare efficiently automates key tasks, such as auto invoice matching and intelligent transaction processing, resident and client portals, streamlined billing and debt management processes, easy to read statements, out-of-the-box industry reporting, and real-time insights into enterprise-wide information.
The great thing about the transformative power of technology, is that allows facilities to focus more on the people they care for, and elevate the level of care they provide, with many benefits along the way.
Whether it’s finding efficiencies through leveraging new software features or unleashing new data insights and improving security and compliance with privacy requirements, TechnologyOne is proud to be part of the aged and community care sector, and support providers on their digital transformation journeys.
Vanessa Devine, Industry DirectorHealth and Community Services, TechnologyOne www.technologyonecorp.com
Whichever technology provider you choose, make sure they’re passionate about helping deliver better care
ACCPA’s Nursing Transition Programs are designed to attract nurses to a career in aged care, and upskill them for residential and community care settings –so your organisation reaps the benefits.

There are two different 12-month programs for Graduate Registered Nurses and Graduate Enrolled Nurses in their first year of practice, as well as a six-month program for experienced Registered Nurses transitioning to aged and community care for the first time.
Registered Nurse Facilitators are available to support the nurse, their mentor and the partnering organisation, for long-term staff retention.
Programs features include:
Online professional development sessions
Forums and networking opportunities
Organisation-based mentoring
On-the-job learning
Clinical assessment of competency

The next program intakes are in February and August 2023.
Get in touch with us today, to find out how your organisation can benefit.
1300 222 721 accpa.asn.au/nursing
www.employment.agedservicesworkforce.com.au/acttpp_organisation/
For residential care, home care, retirement living and disability operators
Over 450 policies, processes and related forms and templates
Supports best practice and compliance against all relevant standards and legislation Audit program and quality assurance management Real-time reporting and version control
Remaining compliant with changing regulations and legislation has become vital for aged care and disability operators, but it’s hard to manage alone.

An easier way is to use an outsourced quality management and compliance system – slashing the time it takes for recording and reporting.
ACCPA has endorsed two reliable, robust and effective quality systems – so your workforce can focus on the caring, not the paperwork.
For aged care providers and disability operators
Management tool for self-assessment against over 100 relevant standards
Over 500 resources and policy templates to assist with compliance Separate module for governing bodies Saves 80% of work time on compliance reporting
1300 222 721 quality@accpa.asn.au www.accpa.asn.au/quality-compliance
The aged services industry is currently experiencing a substantial transitional shift from relying on the old residential care models of the past into a new era that will be expected to offer more choice, dignity and built quality.
While it was common for some older people to reluctantly accept the available ‘nursing home’ offerings as an inevitable path towards the end of their days, today many older people are planning ahead to find places that they choose in advance of potentially needing physical care.
‘Downsizers’ capture a market that lures people into retirement communities offering a range of lifestyle options which are packaged up with elegantly designed places in areas where they can continue to maintain connections with their communities. The social value of these communities is well understood and sought after, but the potential for ageing in place also underpins the resident’s sense of security and peace of mind.
Many older people won’t need to rely on a high level of physical care as they age, but as we are living longer, many people will eventually need some level of help with daily activities, meals and support and health management.
High care for very frail people or those with advanced dementia will still demand a specific accommodation. In these environments where there are a lot of communal and shared spaces for dining, activities and relaxation, each resident will also have their own personal space in the form of a private suite. The private suite will provide a bedroom and bathroom as a minimum. With the expectations however for greater dignity and respect and to ‘deinstitutionalise’ care environments, it is becoming more common for
developers to present their ‘care suites’ as small apartments.
There are various versions of this accommodation type being considered and explored. In some instances, the care apartments are presented more like a regular apartment off a typical corridor in a multi-storey building.
Residents can receive varying services in their care apartment that are tailored to the needs and requirements of each individual in their own space. These services can be in the form of separate home care packages that can be outsourced or provided on site.
As architects who work very specifically in the aged care and retirement living sectors, Calderflower are seeing a range of different viewpoints around this model. Does it reinvent ‘residential care’ however as a new and potentially larger building type?
If residents, who are frail and very dependent, remain in their care apartment would they be isolated and alone?
Someone moving from their home to a care apartment will be seeking out a like-minded community as well as the appropriate style of accommodation. A positive aspect of residential aged care is the communality of groups which can help alleviate loneliness and isolation, along with the availability of staff. In the absence of the ‘communal living’ concept of residential aged care, where does the sense of community come from in a care apartment style development?
Residents in a care apartment would have the choice of whether to join in activities and have shared meals in a dining room or stay in their unit and enjoy the privacy and amenity of their own space and utilities.
In this sense, it provides more choice and flexibility for residents when they are more mobile and active. As a resident’s care needs increase and they become less mobile and more dependent, they will need to find a way to interact with other residents to maintain social engagement.
The food experience enjoyed in a shared dining room provides a core social hub in most care environments. Mealtimes are highly anticipated, and the presence of quality food and atmospheric ambiance can go far in bringing people together.
The kitchen or food service area can also be designed to be a resident friendly space where cooking as a social activity can be shared and enjoyed with others, even if just as an observer.
The provision of communal spaces such as lounges, reading rooms, craft areas, wellness hubs and allied health services, a bar or club room and garden clubs, pet walking groups and so on, are essential elements needed to bring people together. The absence of these vital areas if the focus is just on accommodation modules and care delivery would defeat the purpose and opportunity of connecting people on a social and supportive level.
The future of care accommodation which supports healthy ageing seems to be becoming more and more of a blended product between independent living units and residential aged care. Confusingly, these are both governed by separate bodies and perhaps bringing these together will help solve some of the challenges in delivering the best type of care accommodation for future ageing communities to embrace.
Lara Calder, Managing Director, Calderflower Architecture www.calderflower.com.au
The focus for architects is no longer just on accommodation, it’s about lifestyle

Small-scale residential age care models are being adopted by providers in varying degrees both in a greenfield context, or when seeking to ‘unbox’ current facilities into smaller housing modules. This adoption is across a continuum starting from a more traditional centralised services model through to what we describe as a pure small house model.
Small-scale residential age care models are being adopted by providers in varying degrees both in a greenfield context, or when seeking to ‘unbox’ current facilities into smaller housing modules. This adoption is across a continuum starting from a more traditional centralised services model through to what we describe as a pure small house model.
In line with the example made famous at De Hogeweyk, a ‘pure’ small house model is where no central services exists and the majority of daily rituals of the house (cleaning, cooking and laundry) are performed in-house with residents. This requires a different staffing model that expands a care role across all disciplines apart from clinical.
Without appropriate planning, current building regulations (Class 9C classification under the National Construction Code) can push an aged care provider down a design pathway with institutional building outcomes, so it’s important to understand that you can shift the paradigm.
Typical traditional models generally take the form of ‘donut’ or ‘H-shaped’ layouts that prioritise maximising bed numbers within a floor plate with expanses of sterile double loaded corridors, rather than focusing on the quality of spaces for residents. Today, we are more regularly challenging these assumptions. By engaging in early discussions with your design team, they can support the deviations you want to achieve.
Many providers are exploring what is now being referred to as a ‘hybrid’ model, which will have elements of daily life engagement with degrees of integrated staffing for a smaller group of residents than found in a traditional aged care home. Integrated staffing describes the merger of traditional segregated roles, for example hotel service and personal care. When unboxing established facilities, we encourage providers to take a ‘minimum viable product approach’. This seeks to establish the minimum viable change required to achieve the desired client experience. Often this may see a small refurbishment with resident involvement. A small but mighty project can set the ball rolling on the future vision and can buy the organisation the time to invest in true transformation.
Often the first change in unboxing is re-establishing satellite dining space in areas decommissioned in the past. This has been done by breaking down serveries and removing
staff-only areas, thus enabling residents and their visitors to access kitchenettes and allow more intimate dining options.
We often hear that providers aren’t exploring small scale models due to the perceived higher operating and capital costs. Our experience suggest that this is only true if a hybrid model leans too closely towards the safety of the traditional. Assuming a greenfield site, as a general rule of thumb we have found there is at least a $5 to $6 per resident per day (PRPD) saving in a pure model when compared to a hybrid on a site. Without the right balance, a business case for a hybrid model will see total staffing to ensure supervision (generally around the pinch point of mealtimes) not being offset by central service cost reductions.
While little formal research has been done on the benefits to residents, observations from providers who have engaged with this model are that is shows great promise. Such observations have included increased social engagement of clients leading to improved functional and nutritional outcomes; improved quality of life indicators; and reduction in adverse events due to unmet needs.
There are many different views on the optimal number of residents per house to maximise client experience. We have found that the right number will depend on your clients’ individual and community context, your staffing culture and your site constraints.

Small scale living by nature, addresses key dementia design principles such as reflecting a familiar domestic scale and promotion of movement, engagement and meaning. By achieving effective visual cueing for residents within their environment small scale design will afford residents an opportunity to live more purposeful moments.
Whether you are looking at building an entirely new home or to spend your refurbishment dollars wisely, there is a lot to unpack in the small-scale opportunities. The key is to clarify your vision for client experience, work with partners that can challenge and guide you away from traditional design, and most importantly adopt a culture that is brave enough to start the journey towards a new future.
Rose Plater, Community, Health and Ageing Manager; Andrew Spilar, Community, Health and Ageing Design & Development Manager, Paynters www.paynters.com.au
Think about the consumer experience when planning your new aged care home or renovationOne of Paynters’ residential aged care living projects.
from a central service hub. This contrasts with a definitive small house model where all those same services are run from within each household. A definite small house model accommodates fully equipped domestic style kitchens and laundries operated by household-based staff, all of whom can provide personal care, cooking and housekeeping duties.
Generally, hybrid models ensue higher operational costs compared to traditional large households of 30 beds or more alongside lengthy corridors. Regardless, Australian Unity chose this model as it allows staff, carers and residents to spend more quality time connecting and cultivating community.
Designing a successful residential aged care development begins with a thorough understanding of the operator’s objectives and their services delivery model.
Australian Unity’s award-winning Better Together® model is a hybrid, combining the best of the small house with traditional aged care models, allowing residents to choose their preferred setting and level of interaction with their community, from quiet reflection in the household sitting nodes, to the wider ranging community spaces.
The Walmsley residential aged care home is nestled within a mature retirement village. In collaboration with the client and consultant team, we developed solutions that supported the Better Together model, site conditions, and staff and residents’ wellbeing.
Accommodating 120 beds grouped into seven households, each household is further grouped into two smaller annexes providing social groupings of small house models. Three households are located on the ground floor, and four on the first.
Communal activity areas are centred on each floor and surrounded by households. Each household accommodates individual living and dining areas, with adjacent intimate sitting nodes providing residents, and their visitors alike, with a choice of interaction ranging from complete privacy in their bedrooms, stepping out into the sitting nodes, socialising with the household in the living and dining areas, or stepping out into communal activity areas to interact with other residents, staff and visitors on that floor.
Other amenities at Walmsley include a café, gymnasium, salon, consulting rooms, and multi-purpose rooms of varying sizes and capacity. The upper-level living spaces extend out to shaded terraces taking in views of the majestic gum trees and established landscape. The expansive light filled atrium provides connection between the levels and, employing a warm palette of complimentary materials, the feature timber staircase overlooks the landscaped gardens.
Though it incorporates features of small house models, the operational model at Walmsley is in effect a hybrid, with meals, laundry and cleaning services delivered to each household
Australian Unity Wahroonga, Team Leader, Mary Fromberger, says, “The Better Together® model gives staff more time to get to know the residents which make them feel as if they’re caring for their families, rather than working, resulting in higher staff satisfaction.”
With complexities of this unique model resolved, other design features fell quickly into place. Spaces were designed to store mobility aids and medical equipment to minimise clinical impressions. Colours, finishes and textures were selected to provide sufficient contrast while remaining soft to avoid the potential for excessive visual stimulation, which is particularly important in memory care. Achieving a home-like aesthetic remained fundamental throughout the interior design. In keeping with current best practices, all rooms accommodate double beds if needed. This addresses a common dilemma where couples are separated, often creating anxiety for residents and their families.
One unique feature in the memory care wing is a quiet communal sitting area designed to resemble a train carriage. Television screens projecting slow moving landscapes are disguised to resemble carriage windows and are placed between bench seats facing one another.
Designed by Foreground Architecture, and built by Ireland Brown Constructions, Walmsley will be completed by the end of 2022 and looks forward to welcoming residents.
Patrick Ong, Principal, Seniors Living; Kerri Pratt, Senior Architect; Jess Hyde, Associate Director, Foreground Architecture www.foregroundarchitecture.com.au
Early architectural sketch of Walmsley residential aged care home.

Providing residents with greater choice in home-style living and community interaction
Passionate about supporting South Australians to live the best life possible as they age, ECH is changing the healthcare landscape with its innovative Care Hotel.
Providing a similar experience to a hotel stay with room service and state of the art technology, the ECH Care Hotel offers a niche aged care respite and recovery service, one that is worth replicating across the country.

An Australian-first opened in 2021, the Care Hotel features sixteen short-stay suites – eight for people transitioning from hospital who may need more frequent care than they can get at home, or people who are recovering from surgery and are not quite ready to go home, and an additional eight for people living with dementia to provide greatly needed respite for carers.
ECH Clinical Nurse Janice Ferrari has been working at the Care Hotel since it opened. An integral part of Janice’s role is to connect with guests at the Care Hotel, their family members and carers, to develop an individualised plan for the care and support each guest will require during their stay.
“For our guests living with dementia, it is important that we make every effort possible to support them to maintain their usual daily routine and minimise any disruptions to it. This helps to avoid guests becoming anxious and unsettled, which are common symptoms that can be experienced by people living with dementia when routine or environment are changed,” says Janice.
The respite area of the Care Hotel enables guests to move around freely, and also houses a purpose-designed hub where guests can share mealtimes. In addition, there is a sensory room that contains a range of tactile, auditory, visual and movement-based experiences that can help when someone might be feeling overwhelmed.
Many of the guests staying in the Care Hotel for respite choose to join in the weekday activities provided through the Social Day Program, which provides meaningful engagement and an opportunity to socialise with small groups of likeminded guests and clients.
The short-stay area of the Care Hotel provides support for guests who may require care following a procedure, an acute hospital stay, deconditioning or loss of confidence (for example, after a fall), in addition to a number of other reasons.
Guests are free to come and go as they please and can be supported further with arranged additional services and therapies throughout the duration of their stay, for an additional cost.
Services include medical and nursing, and a range of allied health care – including physiotherapy, podiatry, occupational therapy, massage, personal training, exercise physiology, dietetics, music therapy, speech pathology – as well as social work.
Meals are also looked after with various options to choose from, and specialist dietary requirements catered for.
Janice says she loves caring for guests and seeing them flourish when they take up the services on offer.
“We have many guests who return to stay on a regular basis, which is true testament to the positive guest experience,” she says.
A stay in the ECH Care Hotel can be charged directly to a Home Care Package or Commonwealth Home Support Program. If the guest is self-funded, they will receive an invoice and they may be able to seek rebates from a private health insurance provider.
Vicky Brett, Marketing Manager, ECH ech.asn.au/carehotel
We are fortunate to work in a purpose-focused industry driven by quality of life and care for the people we support. But your staff don’t work for love alone. Ensuring they are paid accurately and on time is critical in keeping employees motivated and retaining quality staff.
Managing payroll effectively, as well as Residential Claims and Billings, can place a huge burden on small to medium sized organisations in the age services industry. ACCPA can help lighten the load, whilst reducing your overheads.
ACCPA has been delivering payroll services for Member organisations for over 20 years. Our team have a complete understanding of modern and older awards as well as the many varied enterprise agreements.
We offer professional, cost effective and accurate payroll processing and comprehensive reporting for each pay cycle, each month and at end-of-year.

Services include:
As well as payroll services, ACCPA can also provide claims and billing services. Our team can manage your accounting function for you, to make sure you maximise your funding entitlements and your residents or clients are billed correctly.
Accurate. Timely. Cost Effective.
Constructing inclusive environments is being made easier with the help of a new guide from the University of Stirling, which can be downloaded online.
Specialist architects at the University of Stirling, Scotland, are appealing to the construction sector to put dementia design at the heart of new projects.
Lesley Palmer, Chief Architect at the University’s Dementia Services Development Centre (DSDC), is part of the team behind the Environments for Ageing and Dementia Design Assessment Tool (EADDAT) – a new resource launched to help families, businesses, housebuilders and construction professionals make buildings and public spaces more accessible to an ageing population.
Successfully piloted by UK government body, Transport for London and English local authority Kirklees Council, the pioneering tool provides user guides, assessment checklists, case studies and examples of best practice, to support better design for those with dementia.
Ms Palmer said, “The main interest has come from individual families, local authorities and those operating care settings. There’s been a lower uptake from the construction industry –we’d like to see more engagement from housebuilders and those working on public buildings.
“As the global population ages, by 2030 the number of people living with dementia is expected to rise to 78 million, meaning it is more important than ever to ensure we design for everyone, and for the future.
“Research has demonstrated that dementia design can help people live independently for longer and support improved quality of life for those living with dementia.
“Additionally, research tells us that age-friendly environments can help foster healthy and active ageing by building and maintaining cognitive capacities across the course of our lives.”
EADDAT has been created using the most current research on ageing and dementia design. Made up of three tiers – Tier 1 and 2, with Tier 3 still in development – each one reflects the scale of intervention required.
Tier 1 is the entry level, created specifically for those wanting to make small changes to the home or in a small business,
and is available free of charge. Tier 2 covers a wider range of building types and is tailored for the construction industry, businesses, healthcare settings and other local organisations. Ms Palmer continued, “Age-related changes in our sight, hearing and mobility affect how we engage with our environment. For example, changes in our eyes impact on depth perception, glare and ability to distinguish contrast. An age supportive environment would account for these changes and use design to support its users.
“Similarly, cognitive change such as dementia also requires specific environmental changes to be made to ensure the user can remain safe and independent.”
Kirklees Council is the first UK local authority to adopt the guidance and has used it to develop their own dementia design guide.
Councillor Musarrat Khan, Cabinet Member for Health and Social Care at Kirklees Council, said, “While we talk about dementia friendly design, the principles work for everyone. This is very much about inclusive design that works well for people at all stages of life. This design guidance is intended to be used by all of us for everything from major building projects to choosing a new doormat for our own home.
“Incorporating these design principles into every stage of the process is highly cost effective. It costs no more to use a dementia-friendly paint scheme or flooring that creates an inclusive environment than it does to make choices that prevent people from enjoying a building or public space.”

The University of Stirling has a distinct reputation in the field of dementia and ageing, and their international centre for knowledge exchange – the Dementia Services Development Centre (DSDC) –is recognised worldwide the field of dementia design with a strong reputation for supporting society to meet the changing needs of an ageing population.
EADDAT can be downloaded from DSDC’s website (www.dementia.stir.ac.uk/resources).
Sarah Manning, Communications Officer, University of Stirling www.dementia.stir.ac.uk
Take leadership to the next level with ACCPA’s leadership training programs designed specifically for aged care settings.
Whether you’re after an accelerated learning experience or you want to cultivate deep understanding of the core practices of leadership, ACCPA’s training modules will provide the tools and insights to sustain leaders and managers in times of crisis and competition.

Register your leaders for existing courses or arrange for an entire leadership team to benefit from bespoke training tailored to your organisational needs in a confidential in-house setting – the choice is yours.
Online coursework and coaching
Six months
CILCA360 analysis Community of practice and Alumni program
Six two-hour workshops
Three months
Optional CILCA360 analysis Option to ‘pick and pack’ or register for the set
Both programs are ideal for emerging as well as established leaders, and discounts are available for ACCPA Members.
Reach out today and secure your future. We’re here to help.
This year smith+tracey is celebrating being 75 years. During this period we have developed a major presence and awareness within the seniors living, aged care, community and education sectors.
In 1948, Des Smith and Dan Tracey set out to create an architectural practice recognised for its design of community and its sense of longevity. Their ethos was about ‘people’ engagement, which formed the foundation of lifelong friendships and acquaintances. This created a collaborative team of like-minded professionals striving to achieve and to develop trusted long-lasting client relationships.
Our origins started in Melbourne, however, our people centred design, our long-term networks, and valued repeat clients have enabled smith+tracey architects to create valued projects nationally. Our culture of learning harnesses the energy and enthusiasm of our passionate team and ensures individual knowledge becomes our collective strength.


As we move forward our team continues to preserve our design principals to support and enhance livable environments for our aging population, carer workplaces and a variety of community focused built outcomes providing opportunities to gather, recreate, meet, grow, celebrate, reflect and share life’s values. Email us at info@smithtracey.com.au or call on 03 8808 6444

www.smithtracey.com.au
The Aged Care Reform train keeps chugging in terms of consultation and laying out the roadmap. To thrive in the next wave, Providers must get five things front and centre when it comes to consumer-facing risk.
1. Understand clearly which consumers experience the greatest degree of risk (harm-inducing) and build these into your business systems and people awareness systems.
This means being able to determine consumer vulnerability.
a. Living on their own
b. Rural and remote with limited-service options
c. Few or no family or friends
d. Cognitive impairment and are unable to problem solve or ‘speak up’ for themselves
e. Have responsive behaviours which may impact on are provision (e.g. aggression, sexual disinhibition, purposeless wandering)
f. Links to any of the nine Special Needs groups as outlined in the Aged Care Act 1997
2. Understand the foundations of ‘capacity and substitute decision making’ for each consumer. No health and aged care system will ever support ‘consenting to neglect’.
Providers will need to ramp up consumer health literacy and awareness and shift to a rights-based approach built around consumer needs, goals and preferences.
Without a doubt, digital transformation has significantly benefitted the RAC industry by improving operational efficiencies, accountability, regulatory compliance, and most crucially resident experiences.
However, given the recent high-profile security breaches, Alexys encourages all Aged Care facilities to urgently examine their current cybersecurity posture and develop a strategy that aligns with the 2022 Security Legislation Amendment (Critical Infrastructure Protection) Act

The importance of such a review cannot be overstated, whilst no CI can ever be 100% guaranteed against malicious

3. Have solid processes for clinical risk (High impact/ High Prevalent risk) – the main focus ones include (irrelevant of program type);
a. Pain Management
b. Falls prevention and management
c. Skin Integrity and pressure injury prevention and management
d. Complex care risks including (not limited to) diabetes, chronic disease, dementia affecting the ability to navigate dignity of risk decision making
e. Nutrition and hydration
4. Consumer deterioration recognition and response systems – very clear clinical pathways which are easy to follow and execute
5. Policy and practices that enable the entire workforce to recognise risks of neglect, abuse and exploitation and have clear processes for the escalation of those risks which include appropriate control measures.
cyber-attacks, it is incumbent on all facility operators to ensure secure, reliable, and uninterrupted IT services.
Australia’s Alexys is at the forefront of risk mitigation through its early adoption of Zero Trust Architecture within its award-winning Aptus nurse call solutions. ZTA, as the name implies, totally eliminates implicit trust, instead validating each stage of every digital transaction across an IP network delivering a substantially reduced vulnerability to breaches by cybercriminals.
www.alexys.com.au
NeRA Cloud is the next evolution of resident agreement software, offering providers sophisticated features in a more connected, productive and secure environment.
Introduced in 2006, NeRA software set the industry benchmark by transforming the resident agreement generation process. NeRA still plays a pivotal role in helping hundreds of providers produce compliant legal agreements successfully.
The move to cloud technology marks the start of a new era. Providers can access data securely from anywhere, using either a smart device or computer. Combined with advanced functions powered by cloud technology, NeRA Cloud will have a positive impact on workplace efficiency, outcomes for residents and the provider’s bottom line.
To look at how you can keep your aged service moving forward using NeRA Cloud, visit www.e-tools.com.au or contact e-Tools Software to schedule a free online demonstration on 03 9573-3277.
Industry icon evolves and enters a new era as NeRA Cloud, with features that greatly improve the resident agreement process
“Bolton Clarke provides independent living services through at-home support, retirement living and residential aged care in Queensland, New South Wales and Victoria. In early 2022, the newest retirement living facility, Europa on Alma, opened in St Kilda, Melbourne. The site, designed in accordance with the Liveable Housing Australia guidelines, is fitted for quality of life, including cinema, library, conservatory style
dining as well as gym. The gym is fitted with air-based HUR equipment, to provide safe, yet efficient training to everyone. The allied health team was consulted in the design and the physiotherapists, together with site manager Guy Marinucci, are keen to welcome everyone to train.“
Visit https://www.huraustralia.com.au/
At its most basic level, an air purifier is only going to perform as well as the filters inside.
When filtering viruses from the air, you need to select an air purifier with a medical-grade HEPA filter. Medical-grade refers to top-tier H13 or H14 efficiency-rated filters that will capture a minimum of 99.95-99.99% of particles @ 0.3 microns (PM 0.3) or larger in size. These are the same filters relied upon in infection control isolation rooms and operating theatres.
For 20 years, InovaAir has provided Australian made air purifiers designed to improve indoor air quality and safety.
InovaAir® purifiers only use H13 medical-grade HEPA filters, providing up to 3 years between changes and guaranteed efficiency for the life of the filter.
For further information visit www.airclean.com.au or call 1300 137 244.
The Australian aged care industry is working under unprecedented pressure in a highly regulated environment, as we negotiate COVID-19 - resulting in a fatigued and depleted workforce with little time for education and training.
Registered Training Organisation VERTO’S clients and contacts have revealed that the types of common issues aged care providers are currently facing include:
• Site assessments as part of the Aged Care Quality and Safety Commission (ACQSC) Standards
• Risk of non-compliance or even sanctions from above assessments
• High turnover of staff
• Lack of time allocated to quality staff training
• No staff training aligned to ACQSC Standards.
In response, VERTO has developed a range of educational resources that address the above issues, and:
• Are mapped to ACQSC) Standards
• Written specifically for residential aged care and community home care facilities
• Are designed for face-to-face delivery
Is your organisation at risk for an ‘unmet’ compliance in your accreditation site audits?
Do you want to be prepared for the new ACQS and their focus on wellbeing, diversity, culture and multifaith practices?
Meaningful Ageing Australia supports providers to embed the practices and services essential to ensure high quality
• Include a facilitator guide for team leaders, educators and registered nurses to deliver
• Include exercises and/or case studies to ensure understanding
• Are supplemented with e-learning to embed and re-enforce learning
• Are written to be concise and don’t require participants to be off the floor, absent or backfilled
• Provide a solution to the “gap” in knowledge between the Certificate III and IV curriculum when compared to the ACQSC Standards
• Can be displayed for reference and re-used
• Can be personalised with write on/rub off capabilities. Additional to the above suite of resources, VERTO continues to offer Certificate III in individual Support (Ageing and Disability) and Certificate IV in Ageing.
Contact Darren (0429 834 705) or Danielle (0418 865 584) to discuss how VERTO can tailor options to suit your needs. Alternatively, more information can be found by visiting https://www.verto.org.au/aged-care-resources.
outcomes for aged care consumers, their relatives and their community.
Our practical resources and professional development opportunities build your staff’s capability to recognise the need for spiritual care and be able to respond with confidence and authenticity.
Contact admin@meaningfulage.org.au for more information about how we can help.
VERTO recognises the tremendous effort of the aged care sector to provide high levels of care and service in a highly regulated environment. In 2019, The Royal Commission into aged care introduced eight quality standards with 42 requirements within these, and continue to release findings and action items for the sector.


VERTO has created an education solution related to the Aged Care Quality and Safety Commission Standards for residential aged care and home and community care.
Each kit contains a set of A2 posters, aligned to the standards, packed with information and a short activity. There is a facilitator guide and an e-learning component to ensure all your training needs are covered. This will provide the tools for ongoing learning and development in short manageable sessions. Some of the resources features include:
Content
Content is easy to understand and translatable to practice.
Resources
Design
Is bite sized learning.
Support
The tools support the onsite team to take ownership of education locally.
The information equally available and deliverable across all shifts.
The train the trainer model works to disseminate this information.
Content based on ACQSC standards and gaps in current Cert III Curriculum.
Poster + practical exercises. A2 PVC-write on/rub off.
– Greta Papps today to discuss how these resources can assist you! Phone 0419 704 058 or email GPapps@VERTO.org.au
VERTO is an RTO that also offers Certificate III and Certificate IV in Individual Support (Ageing and Disability) full qualification training For more information call 1300 483 786 or visit www.verto.org.au
Assistance is offered to support the site to embed teaching and learning as business as usual.
to preventuidconsistency,providingtheconsumerwiththerequiredassistance manageachokingincidentand achokingincidentoccurs
Whatisaspirationpneumonia? Aspirationpneumoniaoccurswhenfood,saliva, uidsorvomit

weknowwhat
are currentlyServiceswillhaveshortlyhaveSIRSintroduced.Legislations beingapproved Parliament. WithintheSIRSschemeis categoryneglect.Theexamples neglectincludewithholdingpersonalcare,nottreatingwoundsorinsufficient assistanceduringmealtimesasexamples.
swallowsomethingandstarted
airway.Theepiglottiswillsnapshut

hasdetectedthatsomethingotherthan
thebody’sresponsetohavingaforeign
lungs.Thisleadstolungirritation(coughing),infection(fever)anddecreasedabilitytocreateoxygenneededtolive.
This form of group learning gives confidence to staff to further their education and training with formal qualifications.
Facilitator guide for the presenter. Supporting resources and feedback form linked by QR code.
 Source: Aged Care Quality and Safety Commission website agedcarequality.gov.au The copyright in this image belongs to the Commonwealth. Its use does not constitute an endorsement by the Commission and is for reference purposes only.
Source: Aged Care Quality and Safety Commission website agedcarequality.gov.au The copyright in this image belongs to the Commonwealth. Its use does not constitute an endorsement by the Commission and is for reference purposes only.