Once, you’d start your day with a brisk walk around the neighborhood. But now, even the thought of navigating stairs feels daunting. The cramping, burning sensation in your legs has worsened over time, leaving you uncertain about its cause.
These painful symptoms, including tingling and numbness in your legs and feet—particularly common in those with diabetes—might indicate either peripheral neuropathy or peripheral artery disease. If you’re struggling with any of these sensations, it’s crucial to consult your doctor. Together, you can explore the possibility of these two progressive disorders. Here’s a comprehensive guide to understanding the differences between peripheral artery disease and neuropathy.
Understanding Neuropathy
Peripheral neuropathy occurs when one or more peripheral nerves are damaged. Peripheral nerves are located outside of the brain and spinal cord. When these nerves are damaged, they can lead to sharp pain, numbness, and weakness in the extremities. If diagnosed with neuropathy, your doctor may recommend over-the-counter medication or in some cases, surgery.¹
Symptoms of Neuropathy
- Difficulty walking
- Burning sensations
- Cramping or general achiness
- Lack of feeling, tingly, or numbness in the legs/feet
- Reduced coordination or balance
- Difficulty sleeping due to leg or foot pain
Peripheral neuropathy is considered to be a progressive disorder. The symptoms may affect your feet and hands first but then make their way up into your legs and arms.²
Neuropathy Diagnosis: Taking Charge of Your Health
While peripheral neuropathy can be challenging to treat, especially in advanced stages, early diagnosis is crucial. The sooner the cause is identified, the better the chance of managing symptoms and preventing complications.
A thorough diagnosis for neuropathy typically involves several steps:
- Detailed discussion: Your doctor will discuss your medical history, current symptoms, and lifestyle habits.
- Physical examination: This may include testing reflexes, muscle strength, and sensation in your limbs.
- Diagnostic tests: Depending on the suspected cause, your doctor might recommend:
- Blood tests: to check for vitamin deficiencies, diabetes, or autoimmune conditions.
- Electrodiagnostic tests (EMG/NCS): These measure nerve and muscle function to assess nerve damage.
- Imaging tests (MRI scans): These can help identify nerve compression or other abnormalities.
Additionally, due to the lack of feeling in your legs or feet, you may miss signs of an infection including small wounds. This can become quite serious, resulting in amputation, if not treated in a timely manner. If you notice slow or non-healing wounds on your foot, it’s crucial to note that peripheral neuropathy is not the only cause. Vascular diseases like peripheral artery disease (PAD) can also cause open wounds to not fully heal, leading to serious infection. High blood sugar in diabetes can damage nerves throughout the body, including those controlling internal organs. This can affect digestion, heart function, how well your kidneys work, and sexual function.
Causes and Risks of Neuropathy
Neuropathy is nerve damage that causes weakness, numbness, and pain, usually in the hands and feet. There are many possible causes of neuropathy, including:
- Diabetes
- Autoimmune diseases
- Vitamin deficiencies: Deficiencies in vitamins B1, B6, B12, and E can all lead to neuropathy.
- Toxins: Exposure to toxins, such as heavy metals and industrial chemicals, can damage nerves.
- Medications: Certain medications, such as chemotherapy drugs and some antibiotics, can cause neuropathy as a side effect.
- Trauma: Physical injury to the nerves can cause neuropathy.
- Inhereditary conditions: Some forms of neuropathy are inherited.
Neuropathy can lead to several complications, depending on the type and severity of nerve damage. Risks include pain; weakness and loss of coordination, muscle wasting, foot ulcers and infections; digestive problems; bladder and bowel control problems; cardiovascular problems and sexual dysfunctions.
Understanding Peripheral Artery Disease (PAD)
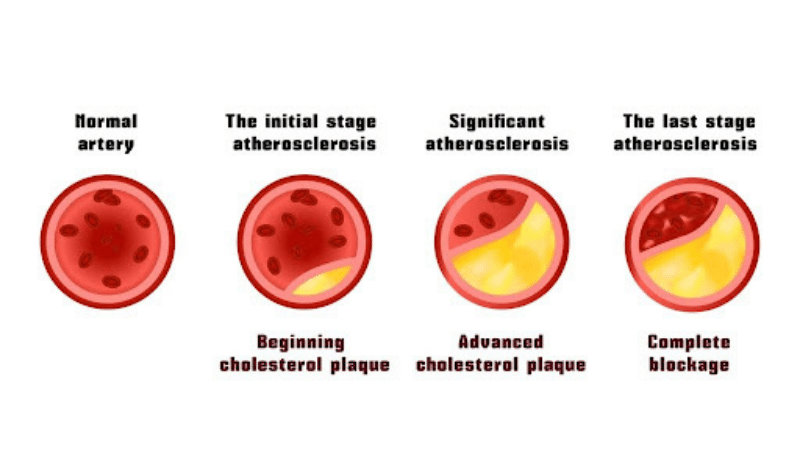
Peripheral Artery Disease, also known as PAD, is a vascular condition caused by a buildup of plaque in the arteries. The plaque buildup narrows the arteries, making it difficult for oxygen, blood, and nutrients to reach the lower extremities.
Symptoms of Peripheral Artery Disease
Peripheral artery disease mainly affects the lower extremities. This is why PAD symptoms can sometimes be mistaken for peripheral neuropathy. However, there are a few outlying symptoms that set them apart; they include:
- Cramps in the thigh, calf, ankle, buttocks, or foot
- Difficulty climbing stairs
- Fatigue or achiness in the legs
- Slow or non-healing wounds on the leg, ankle, or foot
- The temperature of one leg is cooler than the other
- Leg hair loss or poor toenail growth
- Numbness or weakness in the legs
- Pain that stops at rest
- Paleness or blueness in one or both legs
PAD Diagnosis
Unfortunately, diagnosing PAD isn’t always easy. Depending on the individual’s case and severity of the condition, some patients experience little to no symptoms. At USA Vascular Centers, our vascular specialists will use an ankle-brachial index (ABI), ultrasound, or angiography to diagnose PAD. Our team will also examine your legs and arms, looking for specific signs of PAD.
If you’re at risk, are experiencing symptoms, or have a family history of PAD, it’s important to get checked by a specialist. Just like peripheral neuropathy, it’s important to catch PAD in the early stages to prevent further complications.
Causes and Risks of PAD
Peripheral artery disease is a serious medical condition that can impact anyone However, PAD is seen to be more prevalent in men than women. Similarly, individuals over the age of 50 and African Americans are at a higher risk for developing PAD. There are some other common risk factors you’ll want to be mindful of. These include:
- High levels of cholesterol
- History of vascular disease
- Type 2 diabetes
- High blood pressure
- Smoking
Can Peripheral Neuropathy Cause Leg Pain?
One of the most common peripheral neuropathy symptoms is pain in the legs or feet. Neuropathy pain in the feet may start as a tingly feeling but can evolve into numbness. People with peripheral neuropathy symptoms may only have them in one or both feet. Many patients report an increase in neuropathy pain in their feet during the night, which disrupts their sleep.
The nature of the pain can vary depending on factors such as activity levels during the day and the severity of the condition. Some describe it as a stabbing pain, while others experience intermittent discomfort. This discomfort can impede certain activities like walking or climbing stairs. If left unaddressed, diabetic neuropathy may advance to complete numbness and muscle wasting, potentially resulting in immobility.
Seeking medical advice is crucial to explore suitable exercises and stretches aimed at alleviating discomfort associated with peripheral neuropathy in the legs or feet.
The Differences Between Neuropathy and PAD
The primary distinction between neuropathy and PAD lies in their respective effects on the body—PAD affects the arteries, while neuropathy impacts the nervous system. Given their overlapping symptoms, seeking professional guidance is crucial. Both peripheral neuropathy and peripheral vascular disease can pose challenges in self-diagnosis, as symptoms such as leg pain may be vague or difficult to interpret. Keeping a daily record of your symptoms can provide valuable insights for your specialist.
To consult an experienced vascular specialist about your pain or symptoms, call 888.773.2193 or schedule an appointment online.
The Role of Diabetes in Both Conditions
The common denominator of peripheral neuropathy and peripheral vascular disease is diabetes. While peripheral neuropathy may weaken your arterial walls, peripheral artery disease makes them rough, allowing plaque to accumulate. If you think either of these conditions causes your diabetic leg pain, discuss it with your doctor and get tested. People with diabetes should communicate regularly with their doctor, work to lower their blood sugar, as well as actively decrease their blood pressure and cholesterol levels.
Peripheral neuropathy and peripheral vascular disease can significantly impact your quality of life by diminishing mobility. Embracing a sedentary lifestyle can accelerate the progression of both conditions. Upon receiving a diagnosis of PAD or peripheral neuropathy, your doctor can formulate an appropriate treatment plan tailored to your needs.
FIND A VASCULAR CENTER NEAR YOU
Treatment Options for PAD
Treatment options for peripheral artery disease vs. neuropathy vary. If you’re diagnosed with PAD, we recommend booking an appointment with a vascular specialist to discuss your treatment options before your symptoms worsen. If left untreated, PAD can impact your mobility and increase your risk of heart attack, stroke, or amputation. At USA Vascular Centers, we offer three different minimally invasive treatments. These include:
- Angioplasty: Pushes the plaque build-up against the artery walls by inflating a balloon-tipped catheter inside the affected artery.
- Stent placement: After an Angioplasty, a mesh stent is placed inside the affected artery to keep it open.
- Atherectomy: Physically removes the plaque from the body with a laser or tiny blade.
For neuropathy, your medical provider may recommend certain medications or pain relievers. Surgery or physical therapy might be needed, depending on the severity of your condition.
As you can see, the differences between neuropathy and PAD aren’t always clear. Thankfully, both of these conditions can be treated easily.
If you’re living with PAD or neuropathy and walking has become difficult, it’s recommended to get tested. At USA Vascular Centers, we diagnose and treat peripheral artery disease through minimally invasive treatments. If you’re not sure whether vascular disease or neuropathy is behind your leg pain, our specialists can help. Give us a call at 888.773.2193 or schedule a consultation online.
Sources Cited
- Peripheral neuropathy. (2021, August 8). Johns Hopkins Medicine.
- Peripheral neuropathy – Symptoms and causes – Mayo Clinic. (2023, September 2). Mayo Clinic.