A glitch in ‘gatekeeper cells’ slowly suffocates the brain
 Breakdown of unique cells that wrap around blood vessels in the brain leads to neuron deterioration, possibly influencing the development of Alzheimer’s
Breakdown of unique cells that wrap around blood vessels in the brain leads to neuron deterioration, possibly influencing the development of Alzheimer’s
Contact: Zen Vuong at (213) 300-1381 or zvuong@usc.edu
Abnormality with special cells that wrap around blood vessels in the brain leads to neuron deterioration, possibly affecting the development of Alzheimer’s disease, a USC-led study reveals.
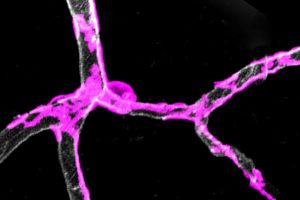
“Gatekeeper cells” called pericytes surround blood vessels, contracting and dilating to control blood flow to active parts of the brain.
“Pericyte degeneration may be ground zero for neurodegenerative disorders like Alzheimer’s disease, ALS and possibly others,” said Berislav Zlokovic, senior author of the study and director of the Zilkha Neurogenetic Institute at the Keck School of Medicine of USC. “A glitch with gatekeeper cells that surround capillaries may restrict blood and oxygen supply to active areas of the brain, gradually causing neuron loss that might have important implications for Alzheimer’s disease.”
Published on Jan. 30 in Nature Neuroscience, this was the first study to use a pericyte-deficient mouse model to test how blood flow is regulated in the brain. The goal was to identify whether pericytes could be an important new therapeutic target for treating neuron deterioration.
“Vascular problems increase the risk of cognitive impairment in many types of dementia, including Alzheimer’s disease,” said Kassandra Kisler, co-first author and a research associate at the Zilkha Neurogenetic Institute. “Pericytes play an important part in keeping your brain healthy.”
A closer look at the mouse models
Pericyte dysfunction suffocates the brain, leading to metabolic stress, accelerated neuronal damage and neuron loss, said Zlokovic, holder of the Mary Hayley and Selim Zilkha Chair in Alzheimer’s Disease Research.
To test the theory, researchers stimulated the hind limb of young mice deficient in gatekeeper cells and monitored the global and individual responses of brain capillaries, the smallest blood vessels in the brain. The global cerebral blood flow response to an electric stimulus was reduced by about 30 percent compared to normal mice, denoting a weakened system.
Relative to the control group, the capillaries of pericyte-deficient mice took 6.5 seconds longer to dilate. Slower capillary widening and a slower flow of red blood cells carrying oxygen through capillaries means it takes longer for the brain to get its fuel.
As the mice turned 6 to 8 months old, global cerebral blood flow responses to stimuli progressively worsened. Blood flow responses for the experimental group were 58 percent lower than that of their age-matched peers. In short, with age, the brain’s malfunctioning vascular system exponentially worsens.
“We now understand the function of blood vessel gatekeeper cells is to ensure adequate oxygen and energy supply to brain cells,” said Amy Nelson, co-first author and a postdoctoral scholar at the Zilkha Neurogenetic Institute. “Prior to our study, scientists knew patients with Alzheimer’s disease, ALS and other neurodegenerative disorders experience changes to the blood flow and oxygen being supplied to the brain and that pericytes die. Our study adds a new piece of information: Loss of these gatekeeper cells leads to impaired blood flow and insufficient oxygen delivery to the brain. The big mystery now is: What kills pericytes in Alzheimer’s disease?”
The research was supported by the National Institutes of Health, the National Natural Science Foundation of China and the American Heart Association.
Scientists at the Zilkha Neurogenetic Institute, the USC Mark and Mary Stevens Neuroimaging and Informatics Institute at the Keck School of Medicine and other collaborators are already working to further this line of research, scanning the brains of people who are genetically at risk for Alzheimer’s. They are also collecting cerebral spinal fluid and blood for analysis of vascular damage, including injury to pericytes.
# # #
ALZHEIMER’S AND AGING RESEARCH AT USC
USC has more than 70 researchers dedicated to the prevention, treatment and potential cure of Alzheimer’s. The memory-erasing illness is one of the greatest health challenges of the century, affecting 1 in 3 seniors and costing $236 billion a year in health care services. USC researchers across a range of disciplines are examining the health, societal and political effects and implications of the disease to improve health across the life span.
Home to an Alzheimer Disease Research Center funded by the National Institute on Aging, USC is one of the top recipients of NIA research grants. The NIA leads funding of research activities on Alzheimer’s, dementia and other age-related diseases and has nearly doubled its investment in USC research in the past decade.
ABOUT THE KECK SCHOOL OF MEDICINE OF USC
Founded in 1885, the Keck School of Medicine of USC is among the nation’s leaders in innovative patient care, scientific discovery, education, and community service. It is part of Keck Medicine of USC, the University of Southern California’s medical enterprise, one of only two university-owned academic medical centers in the Los Angeles area. This includes the Keck Medical Center of USC, composed of the Keck Hospital of USC and the USC Norris Cancer Hospital. The two world-class, USC-owned hospitals are staffed by more than 500 physicians who are faculty at the Keck School. The school today has more than 1,500 full-time faculty members and voluntary faculty of more than 2,400 physicians. These faculty direct the education of approximately 700 medical students and 1,000 students pursuing graduate and post-graduate degrees. The school trains more than 900 resident physicians in more than 50 specialty or subspecialty programs and is the largest educator of physicians practicing in Southern California. Together, the school’s faculty and residents serve more than 1.5 million patients each year at Keck Hospital of USC and USC Norris Cancer Hospital, as well as USC-affiliated hospitals Children’s Hospital Los Angeles and Los Angeles County + USC Medical Center. Keck School faculty also conduct research and teach at several research centers and institutes, including the USC Norris Comprehensive Cancer Center, the Zilkha Neurogenetic Institute, the Eli and Edythe Broad Center for Stem Cell Research and Regenerative Medicine at USC, the USC Cardiovascular Thoracic Institute, the USC Roski Eye Institute and the USC Institute of Urology.
In 2016, U.S. News & World Report ranked Keck School of Medicine among the Top 40 medical schools in the country.
For more information, go to keck.usc.edu.
Image: Pericytes, gatekeeper cells, are wrapped around capillaries in the cortex of a mouse brain. (Amy Nelson/Keck School of Medicine of USC)
