Abstract
Listeria monocytogenes is a main etiological factor of listeriosis, spread mainly by food products. In recent years, an increasing number of patients with listeriosis and an augmentation in L. monocytogenes antibiotic resistance, e.g. to penicillin and ampicillin, has been reported. The aim of the study was to characterise the L. monocytogenes strains isolated from fish-processed food products. Species identification, based on the multiplex-PCR reaction, was performed, and the genetic similarity of the isolates was analysed with the RAPD technique. The strains, in the form of planktonic cells and a biofilm, were subjected to drug-susceptibility analysis, and the effect of disinfectants on the bacillus cells was evaluated. All of the analysed strains were of the Listeria monocytogenes species. Three genetically distant strains were detected, i.e. Lm I, Lm II and Lm III. Approximately 66.6% penicillin-resistant and 66.6% cotrimoxazole-resistant strains were found. No erythromycin-resistant strain was detected. The Lm II strain was simultaneously resistant to four antibiotics, i.e. penicillin, ampicillin, meropenem and cotrimoxazole. The strongest biofilm was formed on aluminium foil and the weakest on rubber. The tested disinfectant antibiofilm effectiveness was related to the type of surface. The most effective agent was paracetic acid and hydrogen peroxide (elimination rate 5.10–6.62 log CFU × cm−2 and 5.70–7.39 log CFU × cm−2 after 1- and 5-min exposure, respectively) and the least—sodium hydroxide (elimination rate 0.52–1.20 log CFU × cm−2 and 0.98–1.81 log CFU × cm−2 after 1- and 5-min exposure, respectively). Further studies on a greater number of L. monocytogenes strains are recommended.
Similar content being viewed by others
Introduction
Listeria monocytogenes is a Gram-positive, non-capsular, facultative anaerobic, rod-shaped bacterium (Sauders and Wiedmann 2007). It has the ability to grow in a wide range of pH and temperature conditions, as well as a reduced sensitivity to vacuum conditions and UV radiation (Fontana et al. 2015; Khan et al. 2013). L. monocytogenes is widely distributed in the natural environment, e.g. in the soil, sewage, surface waters and decomposing plant matter (Abdala 2013; Chambel et al. 2007). Food products, i.e. raw meat, fish, vegetables, fruits and dairy products, are a popular source of those pathogenic bacilli (Sauders and Wiedmann 2007). Secondary food contamination results from the bacteria ability to form a biofilm on the surface of equipment used in food processing plants (Colagiorgi et al. 2016; Sokunrotank et al. 2013). Within the biofilm produced, the microorganisms metabolic and physiological processes are regulated by auto-inducing quorum sensing (QS) signalling molecules (Garmyn et al. 2009). In the biofilm structure, the bacilli are characterised by an increased antibiotic- and disinfectant-resistance (Sokunrotank et al. 2013). This results from the biofilm specific structure, which is stabilised by the so-called extracellurar polimeric substances (EPS) that form the biofilm matrix (Sokunrotank et al. 2013). EPS is an important element that protects cells from drying, phagocytosis and the penetration of antimicrobial agents into the inner layer of the biofilm (Abdala 2013; Kołzwan 2011). The increasing resistance of microorganisms enforces the use of various methods of their elimination. Disinfection is one of them. It is performed by using physical or chemical methods. The procedure allows to reduce the number of bacilli to a certain level. The most commonly applied chemical disinfectants are the following: (1) halogens and their derivatives: hypochlorite, chloramine T, chlorine dioxide; (2) iodophors; (3) peroxygen compounds: hydrogen peroxide, peracetic acid; (4) ozone; (5) alcohols: ethyl, propyl, isopropyl; (6) formaldehyde and glutaric aldehyde; (7) surfactants; (8) quaternary ammonium compounds; (9) nitrogen compounds: polyamides; (10) organic and inorganic acids and their derivatives: acetic acid; (11) heavy metal compounds. Depending on the concentration, disinfectants may act bacteriostatic or bactericidally. Disinfectants may cause the following: (1) destruction of the cell wall; (2) damage to the cytoplasm; (3) oxidation of bacteria cell membrane, proteins, double bonds, enzymes, RNA and DNA, as well as sulphhydryl groups to disulphide bridges (hypochlorite and peroxyacids); (4) inhibition of active transport across the cell membrane (quaternary ammonium compounds); (5) protein coagulation and/or inhibition of their synthesis (aldehydes); (6) blocking the active enzyme centers (Baranowska et al. 2014).
The aim of the study was to characterise L. monocytogenes strains isolated from a fish processing plant. Species identification (via multiplex-PCR) and genetic similarity analysis (RAPD-PCR) of isolates were performed. The drug-susceptibility and the effect of disinfectants on the bacteria in both planktonic and biofilm forms were evaluated.
Material and methods
Materiał
The research involved 20 samples of raw material, semi-final and final product obtained from the fish processing plant (sampling in accordance with the PN-ISO 18593 norm) (Polish Norm PN-ISO-18593 2005).
Methods
Detection of L. monocytogenes in food samples
Isolation of L. monocytogenes bacilli from the samples was performed in accordance with the PN-EN ISO 11290-1: 201707 norm (Polish Norm PN-EN-ISO 11290–1:2017:07 2017). The samples were incubated in half-Fraser broth (24 h, 37 °C). Next, 0.1 ml of the suspension was transferred to the Fraser broth (9.9 ml, incubation: 48 h, 37 °C). A surface culture was initiated on the agar substrate for Listeria, according to Ottaviani and Agosti (ALOA) (MERCK), from the potentially positive samples, i.e. for which a black discolouration of the substrate was reported (incubation: 24 h, 37 °C). The incubation was prolonged for another day, if there was no growth after the first 24 h. Plates with green-blue colonies, surrounded by an opaque zone, were used in the further analysis.
DNA isolation
Total genomic DNA was isolated from samples using a Genomic Mini AXE Bacteria Spin column kit (A&A Biotechnology, Poland), according to the manufacturer procedure.
Isolates identification (multiplex-PCR)
The PCR reaction was utilised to identify the isolates (Bubert et al. 1999). Two primer pairs were applied: L1/L2 and LM1/LM2 (Table 1) (Abdala 2013; Leclerq et al. 2010). Each 25 μL reaction volume contained 1 × PCR bufor (Promega); 25 mM MgCl2 (Promega); 10 mMdNTP Solution Mix (Promega); 10 μM of each primer pair (Oligo.pl); 1 U Taq DNA polymerase (Promega); 2 μL template DNA and sterile, double-distilled water to volume. Amplification was performed as follows: one cycle of 2 min at 94 °C for initial DNA denaturation; 30 cycles of 30 s at 94 °C for denaturation, 30 s at 50 °C for annealing and 1 min at 72 °C for DNA extension. The last cycle was followed by a final extension step of 5 min at 72 °C.
The amplified DNA fragments were separated on 1.5% (w/v) agarose gel, in a TBE buffer, and detected by staining with Midori Green (NIPPON Genetics EUROPE gmbH). Molecular weights of the fragments were estimated using a 100–1000 bp DNA molecular marker (A&A Biotechnology, Poland). Listeria monocytogenes ATTC 7644 was used as the reference strain.
Genetic similarity evaluation (RAPD-PCR)
The isolates’ genetic similarity evaluation was performed with the RAPD technique (Random Amplification of Polymorphic DNA) (Park et al. 2012). The reaction was performed using the OPA-11 primer with the 5’–CAATCGCCGT–3′ sequence (Ozbey et al. 2006). Each 25 μL reaction volume contained 1 × PCR bufor with 2 mM MgCl2 (Promega); 200 μM dNTP Solution Mix (Promega); 1 μM single OPA-11 primer (Oligo.pl); 1.25 U Taq DNA polymerase (Promega); 3 μL template DNA and water to volume. Amplification was performed as follows: one cycle of 1 min at 94 °C for initial DNA denaturation; six cycles of 2 min at 30 °C for annealing and 1 min at 72 °C for DNA extension; 35 cycles of 15 s at 94 °C for initial DNA denaturation; 40 s at 37 °C for annealing and 35 s at 72 °C for DNA extension. The last cycle was followed by a final extension step of 10 min at 72 °C.
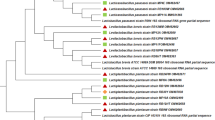
The amplified DNA fragments were separated on 2.0% (w/v) agarose gel, in a TBE buffer, and detected by staining with Midori Green. To evaluate the genetic similarity, a phylogenetic dendrogram was plotted in the CLIQS 1D Pro software (TotalLab). The clustering analysis was performed using the UPGMA hierarchical grouping technique (Unweighted Pair Group Method of Aritmetic Means). Measures of genetic uniformity among recovered individuals were determined using the dice dissimilarity coefficient.
Drug-susceptibility analysis
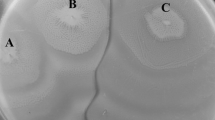
The antibiotic susceptibility of the strains tested was determined using the disk-diffusion method. In the study, the strains’ susceptibility to penicillin (1 IU), ampicillin (2 μg), meropenem (10 μg), erythromycin (15 μg) and cotrimoxazole (1.25–23.75 μg) was evaluated. The prepared antibiograms were incubated at 35 °C for 20 h. After the incubation period, growth inhibition zones around the antibiotic discs were measured. The results were analysed in accordance with the EUCAST ver. 7.0 recommendations.
Determination of the minimum bactericidal concentration of disinfectants
To determine the value of the disinfectant minimum bactericidal concentration (MBC), against the tested L. monocytogenes strains and the L. monocytogenes ATTC 7644 reference strain, dilution series were prepared in hard water of composition compliant with the PN-EN-1276 norm (Krzywicka et al. 1993). Disinfectant concentrations of 0.001, 0.01, 0.05, 0.1, 0.5, 1.0, 2.0% and 0.1, 0.5, 1.0% were prepared for 1- and 5-min exposure, respectively.
A 20 μl sample of the tested strain suspension (0.5 on the MacFarland scale) was placed in the well of a titration plate, and 180 μl of the disinfectant, at the described above concentrations, was added. The disinfectant action was terminated after 1 and 5 min. For this purpose, 20 μl of the sample tested was transferred to 180 μl neutralising solution, i.e. nutrient broth (1000 ml), lecithin (3.0 g l−1), histidine 1 (1.0 g l−1), anhydrous sodium thiosulphate (7.84 g l−1) and Tween 80 (30.0 g l−1) (Krzywicka et al. 1993) and incubated for 2 min at room temperature. Next, 3 μl of the neutralised solution, for each concentration tested, was taken by a multi-channel pipette and cultured on the Columbia Agar with 5.0% sheep blood. The growth on a solid medium was evaluated after 24- and 96-h incubation (37 °C). The disinfectant concentration at which there was no bacteria development was considered as the MBC for a given dilution series.
Biofilm formation by L. monocytogenes strains on various surfaces and the effect of disinfectants on the bacilli in the biofilm
The surfaces tested included sterile elements made of rubber, stainless steel, polypropylene and aluminium foil (size: 10 mm × 20 mm). Suspensions of the tested L. monocytogenes strains and the ATTC 7644 L. monocytogenes reference strain, with a 0.5 optical density on the MacFarland scale, were prepared in test tubes containing 4 ml of sterile brain-heart (BHI) broth (Beton-Dickinson). The surfaces tested were immersed in the suspension and transferred to a fresh sterile BHI broth every 24 h. After 72 h, the surfaces were rinsed twice with buffered saline (0.9% PBS; Avantor). These surfaces were used in evaluation of biofilm formation by examined strains and assesement of antilisterial effectiveness of tested disinfectants.
For the determination of ability to biofilm formation by tested strains, the surface with biofilm was placed in a tube containing 3 ml of PBS. Then sonication was performed using the sonicator Ultrasonic DU-4 (Nickel-Electro Ltd.). After sonication, serial tenfold dilutions of the obtained suspension were made and inoculated on the Columbia Agar medium with 5.0% sheep blood (Becton Dickinson), 100 μl on each. Twenty-four-hour incubation was made at 37 °C in the aerobic atmosphere, and the obtained result was presented as logarithm of the number of colony forming units (CFU) per 1 cm2 of the surface tested.
The influence of four disinfectants, which contained the following: peracetic acid and hydrogen peroxide, quaternary ammonium compounds, sodium hydroxide or sodium hypochlorite as active compounds, was analysed. The surfaces tested, with a biofilm, were placed in disinfectant solutions prepared according to the PN-EN-1276 norm (Polish Norm PN-EN-1276 2000). The experiment included a 0.5% disinfectant concentration for both exposure times. After a given time, the surfaces were immersed in the neutralising solution and then sonicated for 10 min (30 kHz, 150 W). A series of tenfold dilutions was prepared in physiological saline, and a surface culture was initiated on the Columbia Agar with 5.0% sheep blood (bioMerieux); incubation at 37 °C for 24–48 h. The procedure was repeated three times with each strain tested L. monocytogenes strains treated with a solution in which the disinfectant was replaced with hard water, in equivalent volume, and was used as the control. The recovered colonies were counted and expressed as the logarithm of the number of colony-forming units (CFU) per 1 cm2 of the surface tested. Logarithmic declines in the number of L. monocytogenes bacilli after disinfectant action, relative to the control, were calculated.
Additionally, the cell viability in the biofilm was evaluated microscopically, without and after the disinfectant treatment, using the LIVE/DEAD BacLight Bacterial Viability Kit (ThermoFisher).
Statistical analysis
The normality of data distribution was checked, based on the Shapiro-Wilk test, for the calculated logarithmic declines in the number of L. monocytogenes bacilli and the means for all strains tested were calculated. The results were statistically analysed with the two-way analysis of variance (ANOVA), and the comparisons of means were made with Tukey post hoc test (p ≤ 0.05) using Statistica 12.0 PL tools (StatSoft). The surface and disinfectant types were considered as the independent variables, while the logarithmic decline of bacteria number as a dependent variable.
Results
Isolates identification (multiplex-PCR)
The PCR reaction was performed on five isolates (Table 2). All isolates were confirmed to be L. monocytogenes, presence of the hlyA and rrs gene.
Genetic similarity valuation (RAPD-PCR)
The phylogenetic dendrogram of the bacilli tested (Fig. 1) indicates the presence of two major phylogenetic lines. Among the five L. monocytogenes isolates used in the study, three genetically different strains could be found. It was shown that two strains included genetically identical isolates (Lm II + Lm V and Lm III + Lm IV). Two of the most genetically similar strains were Lm I and Lm II. The level of their genetic similarity reached approx. 5.0%. The lowest level of genetic similarity, approx. 1.0%, was found between Lm I and Lm III strains.
Drug-susceptibility analysis
Penicillin- and cotrimoxazole-resitance were the most often reported among the strains tested. Resistance to penicillin (66.6% of strains tested) and cotrimoxazole (66.6%) was found in Lm I and Lm II strains. Resistance to ampicillin (33.3%) and meropenem (33.3%) was found in Lm II strain. There was no erythromycin-resistance reported among the studied population (Table 3). Three susceptibility profiles could be distinguished. The Lm II strain (profile II) was simultaneously resistant to four antibiotics (penicillin, ampicillin, meropenem and cortimoxazole). The Lm III strain was sensitive to all antibiotics tested (profile III) (Table 3).
Determination of the minimum bactericidal concentration of disinfectants
The disinfectant concentration at which no growth of bacteria was observed after further culturing on the disinfectant-free substrate was considered as the MBC for a given series of dilutions. It was found that peracetic acid and hydrogen peroxide were the most effective in inhibiting the bacteria strains growth after 24-h incubation. The peracetic acid and hydrogen peroxide MBC value, during 60-s contact with the disinfectant, was 0.001% with the L. monocytogenes ATTC 7644 reference and Lm III strains and 0.01% for Lm I and Lm II strains. The MBC value increased (0.01%) with the Lm III strain after 96-h incubation. It was reported that the MBC value for 5-min exposure to peracetic acid and hydrogen peroxide, after 24- and 96-h incubation, reached 0.1% for all strains tested. As for the 60-s exposure, the bacilli growth inhibition was observed at 0.01% sodium hypochlorite concentration with L. monocytogenes ATCC 7644, Lm I and Lm III strains, and at 0.05% for the Lm II strain. An increase in the MBC value (0.05%) was observed with the Lm I strain after 96-h incubation. A 0.1% MBC value, after 5-min exposure to sodium hypochlorite, was reported for all strains after 24- and 96-h incubation. As for quaternary ammonium compounds, the bacteria growth inhibition was reported at 0.01% concentration with the Lm II strain and at 0.05% with the remaining strains, for both 24- and 96-h incubation. On the other hand, the MBC value after 5-min exposure to the disinfectant was 0.1% for all strains tested and both incubation periods. It was found that sodium hydroxide was less effectively inhibiting bacilli growth in the biofilm formation. It was reported that the MBC value, after a 60-s exposure to the abovementioned disinfectant, was 1.0% with the L. monocytogenes ATTC 7644 reference and Lm III strains or 2.0% for the Lm I and Lm II strains. As for 96-h incubation, the MBC value increased to 2.0% with the Lm I strain. Growth inhibition after 5-min exposure to sodium hydroxide was found at 0.5% concentration for L. monocytogenes ATTC 7644 reference and Lm III strains and at 1.0% for Lm I and Lm II strains (Table 4).
Biofilm formation by L. monocytogenes strains on various surfaces and the effect of disinfectants on the bacilli in the biofilm
All tested strains formed biofilm on examined surfaces. Regardless of the strain, the highest number of L. monocytogenes was isolated from the biofilm on the aluminium foil and the smallest from the biofilm on the rubber (Table 5). Among the tested strains, the strongest biofilm was formed by the strain Lm I, for which the number of bacilli isolated from the biofilm ranged from 6.90 log CFU × cm−2 on rubber to 7.99 log CFU × cm−2 on aluminium foil (Table 5). In turn, the weakest biofilm was formed by the Lm III strain, for which the number of re-isolated bacteria ranged from 5.94 log CFU × cm−2 from biofilms on rubber to 7.74 log CFU × cm−2 from biofilms on aluminium foil (Table 5).
The obtained results showed differences in the antilisterial effect of disinfectants tested, depending on the active substance contained, surface type and exposure duration (Figs. 2 and 3).
Bacilli number decrease (average for all tested strains) in the biofilm on the tested surfaces after 60-s exposure to various disinfectants (a, b, c, ...—values marked with different letters differ statistically significantly, K—average for all strains initial number of L. monocytogenes (prior disinfection) in biofilm on particular surfaces)
Bacilli number decrease (average for all tested strains) in the biofilm on the tested surfaces after 5-min exposure to various disinfectants (a, b, c, ...—values marked with different letters differ statistically significantly, K—average for all strains initial number of L. monocytogenes (prior disinfection) in biofilm on particular surfaces)
After 1 min exposure, peracetic acid and hydrogen peroxide caused the greatest decreases in the number of cells isolated from the biofilm, i.e. from 5.10 log CFU × cm−2 (rubber) to 6.63 log CFU × cm−2 (stainless steel). The recorded logarithmic decrease in the bacteria number was significantly higher in comparison to all other compounds, regardless of the surface type, only with exception of aluminium foil (Fig. 2). On the other hand, the lowest reduction in the L. monocytogenes bacilli number, recovered from the biofilm after 1-min disinfection, was recorded after applying sodium hydroxide on each surface. The recorded decrease values reached from 0.52 log CFU × cm−2 on aluminium foil to 1.20 log CFU × cm−2 on polypropylene; however, significant differences were observed only with peracetic acid and hydrogen peroxide-based disinfectants on all surfaces, quaternary ammonium compounds on stainless steel and with all tested disinfectants on aluminium foil (Fig. 2).
For sodium hydroxide, the greatest decrease in the L. monocytogenes bacilli number isolated from the biofilm (1.20 log CFU × cm−2), after 1-min contact, was found on the polypropylene surface. In turn, for quaternary ammonium compounds and for sodium hypochlorite, the greatest reductions of L. monocytogenes in biofilm (5.10 and 3.84 log CFU × cm−2, respectively) were obtained on aluminium foil (Fig. 2). For paraacetic acid and hydrogen peroxide, the highest effectiveness against L. monocytogenes (6.63 log CFU × cm−2) was noticed on stainless steel (Fig. 2).
The lowest efficiency of majority of tested disinfectants (without sodium hydroxide) was demonstrated on the rubber surface (Fig. 2). Significant differences in the effectiveness of particular disinfectants, depending on the surface type, were found for the quaternary ammonium-based compounds, acting on the biofilm on rubber vs. stainless steel and aluminium foil and on polypropylene vs. aluminium foil, as well as for sodium hypochlorite acting on the biofilm on aluminium foil vs. rubber and stainless steel (Fig. 2).
Similarly to the 1-min contact, after 5-min exposure to the disinfectant, the highest decline in the cell number, i.e. 5.7–7.39 log CFU × cm−2, was reported for peracetic acid and hydrogen peroxide, regardless of the surface type. A significantly greater logarithmic decrease in the bacteria number was recorded on each surface in comparison to other agents, except the quatery ammoinium compounds acting against biofilm on stainless steel and aluminium foil (Fig. 3). On the other hand, the lowest reduction in the number of bacilli isolated from the biofilm, after 5-min exposure to the disinfectant, was demonstrated for the sodium hydroxide-based agent, for each tested surface. The recorded decrease values reached from 0.98 log CFU × cm−2 (aluminium foil) to 1.81 log CFU × cm−2 (polypropylene). Significant differences in the decrease values were reported for sodium hydroxide vs. other tested disinfectants acting against biofilm on stainless steel and aluminium foil and vs. peracetic acid and hydrogen peroxide on rubber and polypropylene (Fig. 3).
For sodium hydroxide, the greatest decrease in the number of L. monocytogenes isolated from the biofilm after 5-min contact with the disinfectant (1.81 log CFU × cm−2), similarly as for 1-min exposure, was found on the polypropylene. In turn, for quaternary ammonium compounds and and sodium hypochlorite, the best antibiofilm activity (6.02 and 4.63 log CFU × cm−2, respectively) was stated on aluminium foil, just like in case of 1-min exposure (Fig. 3). For peracetic acid and hydrogen peroxide, the greatest decrease in the number of L. monocytogenes isolated from the biofilm (7.39 log CFU × cm−2) was found on polypropylene.
After 5-min, the lowest efficiency of all agents tested against the biofilm of L. monocytogenes was demonstrated on the rubber surface (Fig. 3). Significant differences in the effectiveness of individual disinfectants, in regard to the surface type, were found only for the quaternary ammonium compunds and sodium hypochlorite, acting on the biofilm on aluminium foil vs. biofilm on rubber and polypropylene (Fig. 3). Moreover, the significant differences in the antibiofilm effectiveness were noticed for sodium hydroxide acting on aluminium foil vs. on polypropylene (Fig. 3).
The microscopic observations confirmed the results regarding the microbiocidal effectiveness of disinfectants obtained in classical culturing methods. Exemplary changes in the percentage of live and dead cells in the selected biofilm layer of L. monocytogenes produced on the rubber surface are shown in Fig. 4.
Discussion
In recent years, the number of patients with listeriosis has been increasing. Fresh and smoked fish are considered to be one of the main sources of pathogenic L. monocytogenes (Ertas and Seker 2005; Fallah et al. 2013). The increasing resistance of bacillia to antibiotics, e.g. penicillin and ampicillin, is a serious problem. The present study showed that 66.6% of strains were penicillin- or catotrimoxazole-resistant. It was also found that 33.3% of strains were resistant to ampicillin. Abdollahzadeh et al. (2016) evaluated the susceptibility of L. monocytogenes strains isolated from seafood to eight antimicrobials, including penicillin, ampicillin and trimeroxazole. They found a high-resistance level of the strains tested to penicillin (57.0%) and ampicillin (100.0%) (Abdollahzadeh et al. 2016). Jamali et al. (Jamali and Thong 2014) reported that strains isolated from open fish markets were resistant to penicillin (n = 7/43, 16.3%) and ampicillin (n = 9/43, 20.9%). Opposite results were obtained by Gelbíčová and Karpiškova (2012), who did not report the presence of a penicillin-resistant strain among the isolates tested. Research conducted by Korsak et al. (2012) in the Polish food processing environment showed that all isolates tested were ampicillin-sensitive. On the other hand, Majczyna and Białasiewicz (2006) found that no strain tested was resistant to cotrimaxazole. Approximately 33.3% of the tested population strains were resistant to meropenem. In a study by Ruiz-Bolivar et al. (2011), it was reported that 44.0% of strains were meropenem-resistant. In the present study, no strains with erythromycin resistance were found. Similar results were recorded by Korsak et al. (2012), who did not detect L. monocytogenes strains resistant to erythromycin. Doménech et al. (2015) showed that only two of the 69 samples tested were erythromycin resistant, and they originated from smoked salmon. Research conducted by Jamali and Thong (2014) confirmed the presence of erythromycin-resistant strains (6.3%).
Due to its ability to form biofilm on surfaces of various porosity, e.g. stainless steel, rubber, polypropylene and glass, L. monocytogenes poses a serious threat to the food industry (Borucki et al. 2003). Doijad and Sukhadeo (2015) showed that after 24 h, the tested bacilli strains formed strong biofilms on surfaces used in the food industry, such as stainless steel, ceramic tiles, polypropylene and glass (microscopic examination). Also in the present study, it was shown that the strains formed a biofilm on the tested surfaces: rubber, polypropylene, stainless steel and aluminium foil after 24 h. It was shown that the number of living cells adhering to the surface of stainless steel was lower in comparison to the number of cells inhabiting polypropylene or rubber. The strongest biofilm was formed on aluminium foil surface. Poimeniodou et al. (2016) found that the surface type significantly influenced biofilm formation by L. monocytogenes. They reported that the average population size of biofilm cells on polystyrene (5.6 log CFU × cm−2) was greater than on stainless steel (4.7 log CFU × cm−2). Yun H. et al. (2010) showed that the number of reisolated L. monocytogenes after inoculation was the highest from aluminium foil, what confirmed our results.
Effective disinfection is an important aspect in food processing plants. The increasing resistance of microorganisms to commonly used agents, e.g. based on sodium hypochlorite or sodium hydroxide, is a serious problem. The present study evaluated the effectiveness of four disinfectants against bacilii cells in the biofilm formation. It was found that peracetic acid and hydrogen peroxide, as well as sodium hypochlorite, were the agents, which most strongly inhibited the growth of those organisms. It was reported that the MBC value for the Lm III strain increased (0.01%) after 96-h incubation, 60-s exposure to peracetic acid and sodium hydroxide. The observed increase in the MBC value after 96-h incubation may be due to the presence of damaged cells or cells with a reduced metabolism that needed time to regenerate and multiply. It was shown that the greatest logarithmic decline in the colony count, after the application of peracetic acid and hydrogen peroxide, was recorded on the polypropylene surface. Beltrome et al. (2015) reported that treatments with peracetic acid and sodium hypochlorite were effective in eliminating L. monocytogenes from the polyethylene cutting board used in a food processing plant. Lee et al. (2016), on the other hand, observed the highest antimicrobial activity of 0.5% peracetic acid against L. monocytogenes and S. aureus biofilm isolated from stainless steel surface in dairy plants. They also found that peracetic acid was ineffective against the cells adjacent to the polystyrene surface (Lee et al. 2016). In the other hand, Cabeca et al. (2012) reported a very high sensitivity of L. monocotogenes strains colonising a stainless steel surface to low concentrations of peracetic acid. In the present study, it was shown that sodium hypochlorite effectively eliminated bacilli in the biofilm formation from the surfaces tested, especially from stainless steel. An opposite result was described by Krysinski et al. (1999), who reported the lowest antimicrobial activity of this compound. Also, Chen et al. (2015) found that peracetic acid and sodium hypochlorite were ineffective against the studied microorganisms (L. monocytogenes, S. Typhimurium, E. coli) in the biofilm formation on the stainless steel surface. They found that dodecyl sulfate sodium salt (SDS) was the only agent which effectively eliminated the bacilli. The authors reported that all three pathogens studied could synthesise catalase, which protects the embedded cells, preventing the full penetration of hydrogen peroxide into the biofilm (Chen et al. 2015). In the present research, it was found that the effectiveness of quaternary chemical compounds was surface type-dependent. As for quaternary ammonium compounds, the highest logarithmic decline in the colony count, i.e. 5.01 log CFU × cm−2, 5-min exposure, was recorded for the stainless steel surface, while the lowest, 3.14 log CFU × cm−2, 5-min exposure, on the rubber surface. Poimenidou et al. (2016) found that quaternary ammonium compounds were more effective against the biofilm formed on polystyrene as compared to the one formed on stainless steel. In contrast, Ortiz et al. (2016) reported the resistance of bacilli to quaternary ammonium compounds caused by the long-term use of those particular disinfectants. In the present study, it was found that sodium hydroxide was the least efficient in eliminating L. monocytoges strains. Similar results were reported by Chen et al. (2015), who claim that sodium hydroxide was ineffective in eliminating the biofilm formed by L. monocytogenes, E. coli or S. typhimurium. Common disinfectants, based on sodium hydroxide or hypochlorite, are becoming less and less effective, due to the increasing tollerance of bacilli. The use of optimised concentrations of various disinfectants, carefully selected depending on the surface type, seems to be a recommended solution. Also, the improvement of existing bacteria screening and elimination strategies, or the development of new ones, should be considered (Krysinski et al. 1999).
The increasing number of listeriosis cases and resistance of bacilli to antimicrobials and conventional disinfectants, including those based on sodium hydroxide, is an important public health problem. Major sources of bacilli are food products that are re-contaminated in food industry plants, e.g. at the raw product processing stage. Disinfectants commonly used in processing plants eliminate planktonic biofilm forms, but are not effective with the mature biofilm structure. The results of the present study provide preliminary information on fish contamination with potentially virulent L. monocytogenes strains. Nevertheless, further studies on a greater number of strains isolated from fish processing plants are recommended.
References
Abdala S (2013) Mechanisms of biofilm formation by Listeria monocytogenes. Doctoral Thesis, University of Leicester, pp 1–256
Abdollahzadeh E, Ojagh SM, Hosseini H, Ghaemi EA, Irajan G, Heidarlo MN (2016) Antimicrobial resistance of Listeria monocytogenes isolated from seafood and humans in Iran. Microb Pathog 100:1–5
Baranowska M, Chojnowski W, Nowak H (2014) Disinfection in diaryplants. Nauki Inżynieryjskie i Technologie 4(15):9–22
Beltrame CA, Martelo EB, Mesquitaetet R’z A et al (2015) Adhesion of Listeria monocytogenes to cutting board surfaces and removal by different sanitizers. J Consum Protection Food Saf 10:41–47
Borucki KM, Peppin JD, White D, Loge F, Call DR (2003) Variation in biofilm formation among strains of Listeria monocytogenes. Appl Environ Microbiol 69(12):7336–7342
Bubert A, Hein I, Rauch M, Lehner A, Yoon B, Goebel W, Wagner M (1999) Detection and differentiation of Listeria spp. by a single reaction based on multiplex PCR. Appl Environ Microbiol 65:4688–4692
Cabeca TK, Pizolitto AC, Pizolitto EL (2012) Activity of disinfectants against foodborne pathogens in suspension and adhered to stainless steel surfaces. Braz J Microbiol 43(3):1112–1119
Chambel L, Sol M, Fernandes I, Barbosa M, Zilhão I, Barata B, Jordan S, Perni S, Shama G, Adrião A (2007) Occurrence and persistence of Listeria spp. in the environment of ewe and cow's milk cheese dairies in Portugal unveiled by an integrated analysis of identification, typing and spatial-temporal mapping along production cycle. Int J Food Microbiol 116:52–63
Chen D, Zhao T, Doyle MP (2015) Control of pathogens in biofilms on the surface of stainless steel bylevulinic acid plus sodium dodecyl sulfate. Int J Food Microbiol 207:1–7
Colagiorgi A, Pierluigi Di C, Zanardi E, Ghidini S, Ianieri A (2016) A look inside the Listeria monocytogenes biofilms extracellular matrix. MDPI. Journal 4(22):1–12
Doijad S, Sukhadeo B. Barbuddhe, Sandeep Gargeetet al. (2015) Biofilm-forming abilities of Listeria monocytogenes serotypes isolated from different sources. PLOS One. https://doi.org/10.1371/journal.pone.013704
Doménech E, Jimenez-Belenguer A, Amoros JA, Ferrus MA, Escriche I (2015) Prevalence and antimicrobial resistance of Listeria monocytogenes and Salmonella strains isolated in ready-to-eat foods in Eastern Spain. Food Control 47:120–125
Ertas HB, Seker E (2005) Isolation of Listeria monocytogenes from fish intenstines and RAPD analysis. Turk J Vet Anim Sci 29:1007–1011
Fallah S, Aziz A, Saei-Dehkordi S, Mahzounieh M (2013) Occurence and antibiotic resistance profiles of Listeria monocytogenes isolated from sea food products and market and market and processing environments in Iran. Food Control 34:630–636
Fontana C, Coconelli Pier S, Vignalo G, Saavedra L (2015) Occurence of antylisterial structural bacteriocins gens in meat borne lacticacid bacteria. Food Control 47:53–59
Garmyn D, Gal L, Lemaitre JP, Hartman A, Pivetau P (2009) Communication and autoinduction in the species Listeria monocytogenes. A central role for the agr system. Communicative and Integr Biol 2(4):371–374
Gelbíčová T, Karpiškova R (2012) Outdoor environment as a source of Listeria monocytogenes in food chain. Czech J Food Sci 30(1):83–88
Jamali H, Thong KL (2014) Genotypic characterization and antimicrobial resistance of Listeria monocytogenes from ready-to-eats foods. Food Control 44:1–6
Khan JA, Rathore RS, Khan S, Ahmad I (2013) In vitro detection of pathogenic Listeria monocytogenes from food sources by convencional, molecular and cell culture method. Braz J Microbiol 44(3):751–758
Kołzwan B (2011) Analysis of biofilms—their formation and functioning. Ochrona Środowiska 33(4):3–14
Korsak D, Borek A, Daniluk S, Grabowska A, Pappelbaum K (2012) Antimicrobial susceptibilities of Listeria monocytogenes strains isolated from food and food processing environment in Poland. Int J Food Microbiol 158:203–208
Krysinski EP, Brown LJ, Marchisello TJ (1999) Effect of cleaners and sanitizeres on L. monocytogenes attached to product contact surfaces. J Food Prot 55(4):246–251
Krzywicka H, Janowska J, Tadeusiak B, Zarzycka E (1993) Metoda określania stężeń użytkowych preparatów dezynfekcyjnych. Metoda nośnikowa. Wydawnictwo Metodyczne Państwowego Zakładu Higieny, Warszawa
Leclerq A, Clermont D, Bizet C, Grimont PAD, Le Fleche-Mateos A, Roche SM, Buchriser C, Cadet-Daniel V, La Monnier A, Lecuit M, Allerberger F (2010) Listeria rocourtiae sp. nov. Int J Syst Evol Microbiol 60:2210–2214
Lee SHI, Cappato LP, Corassin CH, Cruz AG, Oliviera CAF (2016) Effect of paracetic acid on biofilm formes by Staphylococcus aureus and Listeria monocytogenes isolated from dairy products. J Dairy Sci 99:1–7
Majczyna D, Białasiewicz D (2006) Characteristic of Listeria spp. bacteria isolated from food products. Med Dośw Mikrobiol 58:119–126
Ortiz S, López-Alonso V, Rodríguez P, Martínez-Suáreza JV (2016) The connection between persistent, disinfectant-resistant Listeria monocytogenes strains from two geographically separate Iberian pork processing plants: evidence from comparative genome analysis. Appl Environ Microbiol 82(1):308–312
Ozbey G, Hassan Ertas HB, FilizKok F (2006) Prevalence of Listerias pecies in camel sausages from retail markers in Aydin province in Turkey and RAPD analysis of Listeria monocytogenes isolates. Ir Vet J 59:342–344
Park S, Jung J, Set C et al (2012) Molecular characterization of Listeria monocytogenes based on the PFGE and RAPD in Korea. Adv Microbiol 2:605–616
Poimenidou SV, Chrysadaakou M, Tzakoniati A, Bikouli VC, Nychas G-J, Skandamis PN (2016) Variability of Listeria monocytogenes strains in biofilm formation on stainless steel and polystyrene materials and resistance to peracetic acid and quaternary ammonium compounds. Int J Food Microbiol 237:164–171
Polish Norm PN-EN-1276 (2000) Chemiczne środki dezynfekcyjne i antyseptyczne- Ilościowa zawiesinowa metoda określania działania bakteriobójczego chemicznych środków dezynfekcyjnych i antyseptycznych stosowanych w sektorze żywnościowym, warunkach przemysłowych i domowych oraz zakładach użyteczności publicznej – Metoda badania i wymagania (faza 2, etap 1). Polski Komitet Normalizacyjny
Polish Norm PN-EN-ISO 11290–1:2017:07 (2017) Mikrobiologia łańcucha żywnościowego – Horyzontalna metoda wykrywania i oznaczania liczby Listeria monocytogenes i innych Listeria spp. - Część 1: Metoda wykrywania. Polski Komitet Normalizacyjny
Polish Norm PN-ISO-18593 (2005) Mikrobiologia żywności i pasz- Horyzontalne metody pobierania próbek z powierzchni z użyciem płytek kontaktowych i wymazów. Polski Komitet Normalizacyjny
Ruiz-Bolivar Z, Neuque-Rico MC, Poutou-Pinales RA et al (2011) Antimicrobial susceptibility of Listeria monocytogenes food isolates from different cities in Columbia. Foodborne Pathog Dis 8(8):913–919
Sauders DB, Wiedmann M (2007) Ecology of Listeria species and L. monocytogenes in natural environment. In: Ryser ET, Marth EH (eds) Listeria, listeriosis, and food safety. Taylar and Francis CRC Pres, BocaRaton, pp 21–45
Sokunrotank S, Iqbal KJ, Sang-Do H (2013) Biofilm formation in food industries. A food safety concern. Food Control 31:572–585
Yun H, Kim B, Jung S, Kruk Z, Kim D, Choe W, Jo C (2010) Inactivation of Listeria monocytogenes inoculated on disposable plastic tray, aluminum foil, and paper cup by atmospheric pressure plasma. Food Control 21:1182–1186
Funding
This research was in part financially supported by the Nicolaus Copernicus University with funds from the maintenance of the research potential of the Department of Microbiology DS-UPB no. 782.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with human participants or animals performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Skowron, K., Hulisz, K., Gryń, G. et al. Comparison of selected disinfectants efficiency against Listeria monocytogenes biofilm formed on various surfaces. Int Microbiol 21, 23–33 (2018). https://doi.org/10.1007/s10123-018-0002-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10123-018-0002-5