Abstract
Background
The aim of this study was to compare long-term clinical and patient-reported outcomes in terms of satisfaction and health-related quality of life (HRQoL) following postmastectomy breast reconstruction using BREAST-Q in patients undergoing implant-based reconstruction, abdominal-based autologous reconstruction, and combined reconstruction (with implant and LD flap or implant and TDAP flap).
Methods
A cross-sectional study was conducted. Patients had undergone delayed postmastectomy breast reconstruction and completed the BREAST-Q reconstruction module. The results were related to the clinical data obtained from the clinic’s patient record system. A 5-year examination was included. Mean scores and standard deviations were calculated. Kruskal–Wallis test, Chi-square goodness of fit test and Chi-square test were used for the statistical analysis.
Results
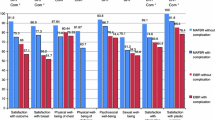
Overall, 110 patients (n = 24 implant, n = 38 autologous, n = 48 combination) were included. Patients with autologous reconstruction reported greater postoperative satisfaction with breasts (p < 0.001), satisfaction with outcome (p < 0.001), psychosocial well-being (p = 0.001), and sexual well-being (p = 0.051).
Conclusion
This study represents a comprehensive long-term examination of postmastectomy breast reconstruction. Autologous reconstruction patients had higher postoperative satisfaction and HRQoL than patients receiving other types of reconstruction despite having more intense oncological therapy and the highest mean number of follow-up surgical procedures.
Level of Evidence III
This journal requires that authors assign a level of evidence to each article. For a full description of these Evidence-Based Medicine ratings, please refer to the Table of Contents or the online Instructions to Authors www.springer.com/00266.


Similar content being viewed by others
References
Tsichlaki A, Fleming PS (2019) Prioritising patients in research and practice:Why and how? J Orthod 46:17–20
Pirro O, Mestak O, Vindigni V, Sukop A, Hromadkova V, Nguyenova A, Vitova L, Bassetto F (2017) Comparison of patient-reported outcomes after implant versus autologous tissue breast reconstruction using the BREAST-Q. Plast Reconstr Surg Glob Open 5:1217
Xiu BQ, Guo R, Yang BL, Zhang Q, Wang J, Su YH, Li L, Ji WR, Zhang YY, Cao AY, Shao ZM, Wu J (2019) Current trends of breast reconstruction after mastectomy in China: a cross-sectional study. Zhonghua Zhong Liu Za Zhi 41:546–551
Cano SJ, Klassen A, Pusic AL (2019) The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstr Surg 123:98–106
Potter S, Mills N, Cawthorn S, Wilson S, Blazeby J (2013) Exploring inequalities in access to care and the provision of choice to women seeking breast reconstruction surgery: a qualitative study. Br J Cancer 109(5):1181–1191
Retrouvey H, Zhong T, Gagliardi AR, PhD Baxter NN MD, Webster F (2019) How patient acceptability affects access to breast reconstruction: a qualitative study. BMJ Open 9(9):e029048
Nelson JA, Allen RJ Jr, Polanco T, Shamsunder M, Patel AR, McCarthy CM, Matros E, Dayan JH, Disa JJ, Cordeiro PG, Mehrara BJ, Pusic AL (2019) Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg 270:473–483
Liu LQ, Branford OA, Mehigan S (2018) BREAST-Q measurement of the patient perspective in oncoplastic breast surgery: a systematic review. Plast Reconstr Surg Glob Open 6:1904
Flanagan MR, Zabor EC, Romanoff A, Fuzesi S, Stempel M, Mehrara BJ, Morrow M, Pusic AL, Gemignani ML (2019) A comparison of patient-reported outcomes after breast-conserving surgery and mastectomy with implant breast reconstruction. Ann Surg Oncol 26:3133–3140
Liu T, Freijs C, Klein HJ, Feinbaum A, Svee A, Lorenzo AR, Liss A, Acosta R, Mani M (2018) Patients with abdominal-based free flap breast reconstruction a decade after surgery: a comprehensive long-term follow-up study. J Plast Reconstr Aesthet Surg 71:1301–1309
Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ (2009) Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 124:345–353
de Blacam C, Healy C, Quinn L, Spillane C, Boyle T, Eadie PA, Connolly EM, O’Donovan D (2016) Is satisfaction with surgeon a determining factor in patient reported outcomes in breast reconstruction? J Plast Reconstr Aesthet Surg 69:1248–1253
Cohen WA, Mundy LR, Ballard TN, Klassen A, Cano SJ, Browne J, Pusic AL (2016) The BREAST-Q in surgical research: a review of the literature 2009-2015. J Plast Reconstr Aesthet Surg 69:149–162
Sugrue R, MacGregor G, Sugrue M, Curran S, Murphy L (2013) An evaluation of patient reported outcomes following breast reconstruction utilizing Breast Q. Breast 22:158–161
Macadam SA, Zhong T, Weichman K, Papsdorf M, Lennox PA, Hazen A, Matros E, Disa J, Mehrara B, Pusic AL (2016) Quality of life and patient-reported outcomes in breast cancer survivors: a multicenter comparison of four abdominally based autologous reconstruction methods. Plast Reconstr Surg 137:758–771
Phan R, Hunter-Smith DJ, Rozen WM (2019) The use of Patient Reported Outcome Measures in assessing patient outcomes when comparing autologous to alloplastic breast reconstruction: a systematic review. Gland Surg 8:452–460
Billig J, Jagsi R, Qi J, Hamill JB, Kim HM, Pusic AL, Buchel E, Wilkins EG, Momoh AO (2017) Should immediate autologous breast reconstruction be considered in women who require postmastectomy radiation therapy? a prospective analysis of outcomes. Plast Reconstr Surg 139:1279–1288
Panchal H, Matros E (2017) Current Trends in Postmastectomy Breast Reconstruction.Plast Reconstr Surg 140(5S Advances in Breast Reconstruction):7-13
Leff DR, Bottle A, Mayer E, Patten DK, Rao C, Aylin P, Hadjiminas DJ, Athanasiou T, Darzi A, Gui G (2015) Trends in immediate postmastectomy breast reconstruction in the United Kingdom. Plast Reconstr Surg Glob Open 3:507
Veronesi P, Ballardini B, De Lorenzi F, Magnoni F, Lissidini G, Caldarella P, Galimberti V (2011) Immediate breast reconstruction after mastectomy. Breast 20(Suppl 3):S104–S107
Chen SA, Hiley C, Nickleach D et al (2013) Breast reconstruction and post-mastectomy radiation practice. Radiat Oncol 8:45
Duxbury PJ, Gandhi A, Kirwan CC, Jain Y, Harvey JR (2015) Current attitudes to breast reconstruction surgery for women at risk of post-mastectomy radiotherapy: A survey of UK breast surgeons. Breast 24:502–512
Rococo E, Mazouni C, Or Z, Mobillion V, Koon Sun Pat M, Bonastre J (2016) Variation in rates of breast cancer surgery: a national analysis based on French Hospital Episode Statistics. Eur J Surg Oncol 42:51–58
Frisell A, Lagergren J, de Boniface J (2016) National study of the impact of patient information and involvement in decision-making on immediate breast reconstruction rates. Br J Surg 103:1640–1648
Heil J, Rauch G, Szabo AZ et al (2013) Breast cancer mastectomy trends between 2006 and 2010: association with magnetic resonance imaging, immediate breast reconstruction, and hospital volume. Ann Surg Oncol 20:3839–3846
Coufal O, Gabrielová L, Justan I, Zapletal O, Selingerová I, Krsička P (2014) Breast cancer patient satisfaction with immediate two-stage implant-based breast reconstruction. Klin Onkol 27:353–360
Tsoi B, Ziolkowski NI, Thoma A, Campbell K, O’Reilly D, Goeree R (2014) Systematic review on the patient reported outcomes of tissue-expander/implant vs autologous abdominal tissue breast reconstruction in postmastectomy breast cancer patients. J Am Coll Surg 218:1038–1048
Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL (2018) Long-term Patient-Reported Outcomes in Postmastectomy Breast Reconstruction. JAMA Surg 153:891–899
Yoon AY, Bozzuto L, Seto AJ, Fisher CS, Chatterjee A (2019) A systematic review of utility score assessments in the breast surgery cost-analysis literature. Ann Surg Oncol 26:1190–1201
Albornoz CR, Bach PB, Mehrara BJ, Disa JJ, Pusic AL, McCarthy CM, Cordeiro PG, Matros E (2013) A paradigm shift in U.S. Breast reconstruction: increasing implant rates. Plast Reconstr Surg 131:15–23
Potter S, Conroy EJ, Cutress RI, Williamson PR, Whisker L, Thrush S, Skillman J, Barnes NLP, Mylvaganam S, Teasdale E, Jain A, Gardiner MD, Blazeby JM, Holcombe C, iBRA Steering Group (2019) Breast Reconstruction Research Collaborative. Short-term safety outcomes of mastectomy and immediate implant-based breast reconstruction with and without mesh (iBRA): a multicentre, prospective cohort study. Lancet Oncol 20:254–266
Ulatowski Ł, Kaniewska A (2015) The use of the diep flap in the modern reconstructive surgery. Pol Przegl Chir 87:472–481
Acknowledgements
The authors would like to thank Jill A. Helms (Stanford University) and Martin Zidek (University of California, San Francisco) for their contributions to this work.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The protocol has been approved by the Ethics Commission, Third Faculty of Medicine, Charles University in Prague.
Informed Consent
For this type of study, formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
266_2020_1926_MOESM1_ESM.tif
Supplementary Fig. 1 (a) Prereconstruction frontal view of a patient after skin-sparing mastectomy; (b) postreconstruction frontal view of a patient after skin-sparing mastectomy (TIFF 6536 kb)
Rights and permissions
About this article
Cite this article
Ticha, P., Mestak, O., Wu, M. et al. Patient-Reported Outcomes of Three Different Types of Breast Reconstruction with Correlation to the Clinical Data 5 Years Postoperatively. Aesth Plast Surg 44, 2021–2029 (2020). https://doi.org/10.1007/s00266-020-01926-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00266-020-01926-5