
Vaccines: a world equipped to combat infectious disease
We want to help develop new vaccines and work out how to use the existing ones in a better way. Discover more about our work on vaccines.
Vaccines are one of our most effective health interventions, but are often misunderstood. In this Q&A, we explain what they are, how they work and why they are important.

We’re protected from infectious disease by our immune system, which destroys disease-causing germs – also known as pathogens – when they invade the body. If our immune system isn’t quick or strong enough to prevent pathogens taking hold, then we get ill.
We use vaccines to stop this from happening. A vaccine provides a controlled exposure to a pathogen, training and strengthening the immune system so it can fight that disease quickly and effectively in future. By imitating an infection, the vaccine protects us against the real thing.
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
It is possible to beat infectious diseases.
We've wiped out one human disease worldwide – smallpox.
We're getting closer to beating others.
Polio cases have dropped by 99% in the last 30 years, saving 16 million people from paralysis.
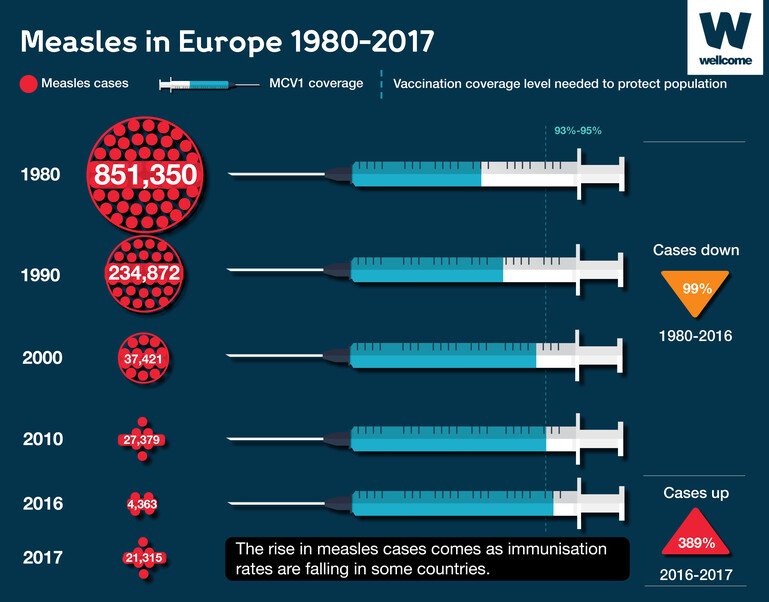
Measles decreased by 84% between 2010 and 2016, saving more than 20 million lives.
This is all thanks to a single medical intervention – vaccines.
But beating disease is not easy.
Around the world there are over 36 million people living with HIV, and malaria and typhoid still harm and kill millions each year.
Diseases like Ebola, yellow fever and cholera can cause deadly epidemics within months.
The next flu pandemic could kill millions, sicken billions, cost trillions.
We need to develop new and better vaccines.
Vaccines are one of the most effective health interventions – our best chance to save lives.
Wellcome is committed to working with experts to improve how vaccines are made and used so that we can beat more diseases.
They protect us from dangerous diseases. In some regions or populations, dangerous diseases are constantly present (endemic). Examples include hepatitis B, cholera and polio. So long as these diseases are around, we need vaccines to bolster our immune systems and protect us from harm.
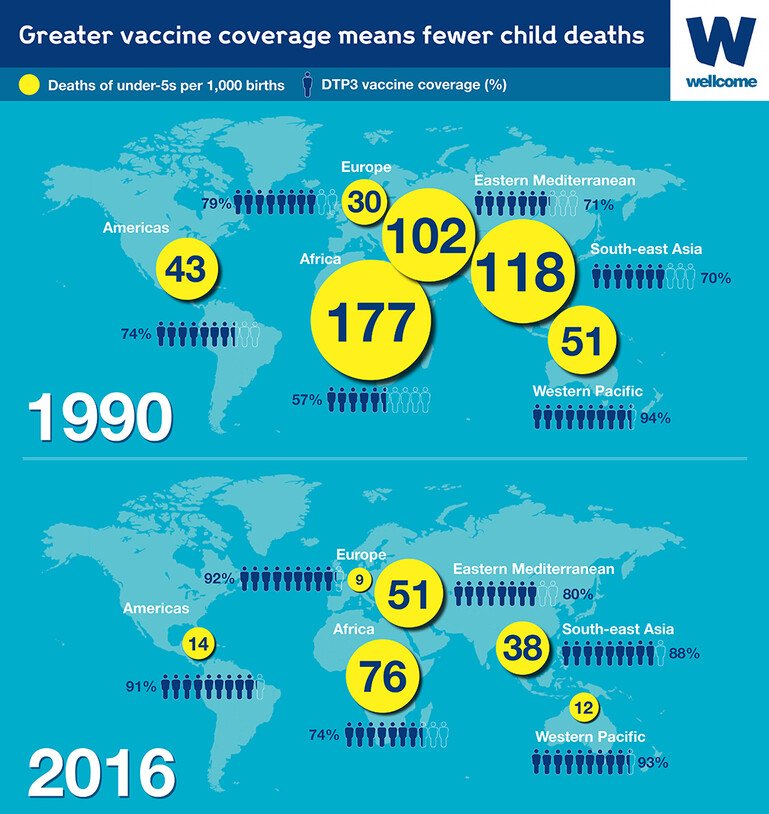
They protect children and the elderly. Our immune systems are strongest in adulthood, meaning that young children and the elderly are particularly susceptible to dangerous infections. By strengthening our immune systems early and late on in life, vaccines bypass this risk.
They protect the vulnerable. If enough of a population is vaccinated, infections can’t spread from person to person, which means that everyone has a high level of protection – even those who don’t have immunity.This is known as herd protection (or herd immunity). It’s important because not everyone can be directly protected with vaccines – some people are unresponsive to them or have allergies or health conditions that prevent them from taking them.
They can help us control epidemics. In a world of denser cities, increased international travel, migration and ecological change, the ability of emerging infectious diseases (such as Ebola) to spread and cause devastation is increasing. Vaccines can be a key tool in managing this threat – but only if we have them ready for diseases when they appear.
They can help limit drug resistance. Medicine relies on being able to treat infectious diseases with antimicrobial drugs, such as antibiotics, but overuse and misuse of these drugs is leading to infections becoming resistant to them. By preventing infections that would require drug treatments, vaccines reduce the opportunity for drug resistance to develop.
They are our most effective health intervention. Vaccines prevent an estimated 2–3 million deaths worldwide every year. But, a further 1.5 million lives could be saved annually with better global vaccine coverage.
Our immune system fights disease by distinguishing between things that belong in our bodies and things that don’t, destroying the latter. Unwanted foreign substances are identified by markers on their surface called antigens.
A vaccine works by exposing the immune system to the antigens from a pathogen, something such as a virus or bacterium that causes a certain disease. When your immune cells encounter these antigens, they mount a response. One cell type – B cells – start making antibodies, which bind to the foreign substance, disable it and mark it for destruction. Other immune cells, known as T cells, attack and destroy cells of the body that have been infected by the pathogen.
At the same time, the body also produces long-lived types of white blood cell – called memory T cells and memory B cells – that remember the antigens that have just been encountered. If your immune system comes across the same antigens again, these memory cells allow you to mount a strong response against that specific pathogen very quickly, so you are much less likely to get ill.
A vaccine contains the antigens from a pathogen, which are needed to provoke the body’s immune response and stimulate the production of antibodies. However, there are different types of vaccine, which deliver antigens in different ways.
Live attenuated vaccines: Some vaccines – such as the BCG (Bacille Calmette–Guérin), which protects against tuberculosis – contain a live version of the whole pathogen. However, in such cases the strength of the pathogen (its virulence) is weakened (attenuated) before it is given, to stimulate an immune response without a full infection. Live attenuated viruses are also used in the measles, mumps and rubella (MMR) vaccine.
Inactivated vaccines: Some vaccines contain an inactive version of a pathogen, one that has been killed – for instance by using heat or formaldehyde. The immune system can still recognise and respond to the pathogen, but as the pathogen cannot reproduce, it poses no risk of infection. Cholera, hepatitis A and rabies vaccines all contain inactivated pathogens.
Toxoid vaccines: The symptoms of some diseases are caused by harmful products of bacteria, known as toxins. Vaccines for these diseases, for example tetanus, use inactivated versions of toxins (called toxoids) to stimulate an immune response.
Subunit vaccines: Other vaccines contain only the antigens of a pathogen that best stimulate a response – these are known as subunit vaccines. By including only the essential antigens, and not the whole pathogen itself, these vaccines are much less likely to cause an adverse reaction, and pose no risk of infection. However, subunit vaccines tend to induce a weaker immune response.
Conjugate vaccines: Finally, some pathogens can be hard for the immune system to identify, and so require a special type of vaccine. Bacteria coated with sugar molecules known as polysaccharides are able to mask the antigenic material on their surface, making it difficult for the immune system to recognise them and mount a response (especially in children). To fight against this, conjugate vaccines are created: the bacteria’s sugar coatings are isolated as subunits and then chemically joined to larger, more readily identifiable carrier proteins. These new constructions, being recognisable, stimulate an immune response that creates antibodies that can also recognise and fight against the coated bacteria in the future.
Other ingredients: As well as these active ingredients, vaccines also contain:
Some vaccines also contain adjuvants: substances such as aluminium compounds that strengthen the immune response to the vaccine’s antigens. These are commonly used in subunit vaccines.
Vaccines may also contain trace elements of substances used during their manufacture: for example, some vaccines are grown using fertilised hens’ eggs and so may contain traces of egg protein, and inactivated vaccines may contain extremely small traces of formaldehyde.
Pressing play on the video above will set a third-party cookie. Please read our cookie policy for more information.
These eggs could save your life.
Eggs.. boiled? Scrambled? Omelette? No... Vaccines.
A vaccine is a very simple means to train your body and to prevent it from being infected by a bacterium or a virus. We are manufacturing here on this site influenza vaccines – seasonal and pandemic influenza vaccines.
We get these eggs from about 14 different farms, spread all over Germany and right into the Netherlands as well.
The manufacturing process of our influenza vaccines starts with the inoculation of the influenza virus into the eggs, followed by an incubation at well-controlled temperatures under well-controlled conditions. During that incubation phase, the influenza virus is multiplying.
In the second stage now, we harvest the allantoic fluid from the eggs. This allantoic fluid now contains millions and millions of copies of influenza virus.
In the next stage, we purify the virus from the allantoic fluid and we also split the virus into small particles and inactivate it chemically in order to prevent it from being able to further replicate.
In the fourth stage, we sterile filter to yield a sterile suspension of purified influenza split virus with each of the four influenza strains we receive from the WHO reference laboratories in order to formulate a quadrivalent vaccine containing two B strains and two different A strains as a base composition for this vaccine.
The manufacture of our bulk antigen takes us about 30 days followed by another 30 days necessary for the formulation, filling, packaging of the vaccine.
Our whole manufacturing process and the success of what we are doing depends on the people we have.
This year we will produce approximately 50 million doses of influenza vaccine, delivering a very safe product which is able to protect people from serious infections.

We want to help develop new vaccines and work out how to use the existing ones in a better way. Discover more about our work on vaccines.
Vaccines generate immunity across the body as a whole, but they can also provoke specific immune responses in specific body areas.
They are most effective if they can stimulate a response where pathogens are likely to invade and harm the body, for instance in mucous membranes. So, to ensure that their action is suitably targeted, the delivery routes of vaccines often mimic the invasion routes of pathogens.
For example, the oral polio vaccine is ingested in order to stimulate an immune response in the lining of the intestines, as this is where the poliovirus ends up and multiplies after entering the body in contaminated food and water.
Intranasal (up-the-nose) delivery of vaccines achieves the same effect, but in the mucous membrane of the nasal cavity. This delivery method is used to combat diseases that need to overcome the nasal mucous barrier in order to infect the body, such as influenza.
However, specific delivery routes are also sometimes necessary to minimise the chances of vaccines having adverse effects on the body. Vaccines containing aluminium-based adjuvants often cause inflammation (granulomas) unless they are injected into muscle tissue, while the BCG vaccine for tuberculosis is injected into the topmost layer of the skin – a process known as intradermal injection – to avoid it causing damage to blood vessels and nerves.
Some vaccines – such as those for yellow fever and measles, mumps and rubella (MMR) – work best when released slowly into the body. For this reason they are injected into the layer of fat between the skin and muscle. The limited blood flow in this area prevents the vaccine from being distributed around the body too quickly. This method is known as subcutaneous injection.
At an individual level, vaccines are very effective at providing protection against certain diseases, though they don’t provide immunity in 100 per cent of cases. Every person’s immune system is different: some people won’t respond to the antigens in a vaccine and therefore won’t become immune.
Rates of effectiveness also vary from vaccine to vaccine: a three-dose course of the inactivated polio vaccine is 99 per cent effective, whereas the effectiveness of typhoid vaccines is only around 70 per cent.
A further complication is that the effects of some vaccinations wear off over time. Two doses of the measles, mumps and rubella (MMR) vaccine will usually provide 20 years’ protection against measles, but the effects of a typhoid vaccine will typically wear off after three years. We currently don’t know why this happens. This is why we have boosters – to ‘remind’ our immune system how to identify certain pathogens and top up our immunity.
At the population level vaccines are highly effective too. They have completely got rid of one disease – smallpox, which was declared eradicated in 1980 – and have brought us close to eradicating others, such as polio.
They can also stop diseases from spreading by creating herd protection. No vaccine is 100 per cent effective, and not everyone in a population will be vaccinated; however, if most people in a population are vaccinated and become immune to a disease, its ability to spread will be vastly reduced. This then protects people without immunity from infection too.
The proportion of the population that needs to be vaccinated to achieve herd protection varies from disease to disease. With measles, for example, 95 per cent of a population must be immune to maintain herd protection.
For those unable to be vaccinated, failure to maintain herd protection can be highly dangerous.
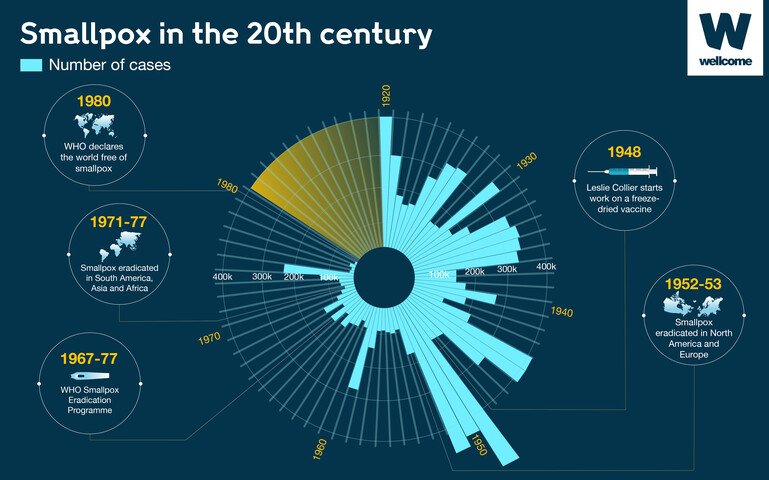
WHO data. A look at smallpox in the 20th century.
Vaccines are very safe in the high-income world – national regulatory agencies govern their testing and manufacture, which ensures that they are safe for human use.
The greatest risks surrounding vaccination are in low-income countries. These risks concern not the vaccines themselves, but their regulation and administration.
Not all national regulatory agencies have the same level of expertise, access to evidence and funding. As a result, some countries may not be able to stop fake vaccines being produced; they may fail to keep the vaccines cold, resulting in spoiled, ineffective vaccines being administered; and insufficient education among those administering vaccines may result in needles being reused, risking the spread of blood-borne diseases such as HIV/AIDS.
Additionally, with live vaccines – which are usually the best at provoking an immune response – there is a very small risk that the live pathogen will mutate to an infectious form. For example, it’s estimated that the live virus in the oral polio vaccine can cause paralysis in about 1 in 2.5 million doses of the vaccine.
It is also recommended that pregnant women avoid taking live vaccines, to prevent live pathogens affecting their unborn child. Likewise, adults recovering from certain illnesses are advised to delay taking certain vaccines until they have recovered.
There are many rumours about negative side-effects of vaccines, which are not just untrue but potentially very damaging. A false claim linking the measles, mumps and rubella (MMR) vaccine to autism in the UK in the 1990s caused levels of vaccination to fall significantly in some parts of the country. This led to a reduction in herd protection, which has resulted in outbreaks of measles and mumps in recent years. Both these diseases can cause encephalitis, a rare but potentially deadly inflammation of the brain.
Vaccines are given to people when they are at risk of contracting a disease. Children – whose immune systems take time to develop – are especially vulnerable, so many countries recommend vaccinating as early as is safe to do so, to make sure they are protected. (Some vaccines are also given to children because they work less effectively in adults.)
Measles, for example, killed 90,000 people globally in 2016, and is a major cause of death among young children. This is why children are given a measles vaccination at an early age.
However, certain diseases become a risk only later in life and so childhood vaccination is not needed. Human papillomavirus (HPV), which can cause cervical cancer, is transferred through sexual contact, so the HPV vaccine is commonly given to girls only once they have reached puberty.
Likewise, before the age of 65 most adults aren’t at risk of becoming seriously ill from influenza. However, as the body ages, its ability to fight flu decreases. Because of this, elderly people are one of five groups that WHO recommends receive seasonal flu vaccination.
Differences and changes in risk explain why vaccine programmes vary from region to region and over time.
Countries set their own vaccine policies, and so these vary around the world, with some countries choosing to make certain vaccines mandatory.
Slovenia, for example, requires that all children are vaccinated against nine key diseases before they start school. Exemption is allowed only for medical reasons, and parents that don’t comply are fined.
On the other hand, a number of other European countries, as well as Australia and Canada, have no mandatory vaccinations. Here, parents or (if old enough) individuals themselves decide.
However, the governments of such countries may offer incentives to make sure that vaccination levels remain high. In Australia, for example, parents receive certain child benefits from the government only if their child has had all of its routine vaccinations.
For some diseases, it’s a question of difficulty.
HIV, for instance, can insert itself into the genetic material of your cells and hide there undetected. Other viruses, like dengue, have multiple strains, which makes it very difficult to create a vaccine that covers them all. With other pathogens, the problem is mutation: continual morphing means that the immune system essentially encounters a new threat every single time, making past exposure count for nothing. This is why the common cold is so problematic.
For other diseases, it’s a question of process: there may already be several promising vaccine candidates in development, but rigorous safety and efficacy testing to make sure they work properly means that an actual approved vaccine is still years away. Developing a vaccine typically takes over a decade.
This is a particular problem with diseases that appear intermittently, as there’s limited scope for testing vaccines to fight them. This is why it’s really important to have vaccine candidates for emerging diseases ready for when outbreaks occur – so that they can be tested, approved and begin protecting people as quickly as possible, before an outbreak can harm too many people. Today we have a vaccine for Ebola only because candidates were ready to test at the beginning of the West African outbreak in 2014 – and even then we were too late to prevent over 11,000 deaths.
Finally, the absence of a vaccine may be down to economics. Vaccine development costs are often quoted in the billions, but many diseases without vaccines disproportionately affect low- and middle-income countries. Pharmaceutical companies have little incentive to invest in treatments that are unlikely to return a profit. This leads to diseases that predominantly affect the low-income world becoming neglected.
In theory, every person should receive every vaccine necessary to protect them from disease. However, not everyone may be able to be vaccinated, for various reasons.
People allergic to trace elements such as egg protein or pork gelatine have to avoid vaccines that are grown using these substances. And some people may be allergic to the antibiotics used in certain vaccines – this is why antibiotics known to often cause allergic reactions, such as penicillin, are generally not used in them.
Others may not be able to take certain vaccines due to pre-existing medical conditions, particularly those that affect the immune system, such as HIV/AIDS, cancer, having had a transplant or being on certain drugs.
But, there are also more contentious reasons. Religious and cultural beliefs lead some people to refuse vaccines, and there’s also hesitancy among some due to beliefs about vaccines being unsafe and/or unbeneficial.
However, the greatest barriers to full vaccine coverage are to do with delivery. One in five children across the world don’t receive their routine childhood immunisations, largely because of difficulties in getting vaccines to them. These children predominantly live in low-income countries.
This may be because of wars or natural disasters disrupting immunisation programmes, or it may be because these children live somewhere where it is difficult to get vaccines to them unspoiled. Vaccines contain biological matter, meaning they often need to be kept cool, which can be difficult in areas with intermittent electricity supplies.
Or, in some countries, it may be because providing all vaccines is too expensive. For the poorest countries in the world, Gavi, the Vaccine Alliance, provides funding assistance for immunisation. However, as its economy develops, a country must move from being financially supported to paying for vaccines itself. In this transitionary period, the costs of providing comprehensive vaccine coverage can sometimes be too great.
Some people delay taking or refuse vaccines, either for themselves or their children, because they do not trust them. This is known as vaccine hesitancy.
Vaccine hesitancy is dangerous. It leaves individuals unprotected against diseases, and also lowers the overall rate of vaccination coverage, threatening herd protection.
Over the past decade or so, vaccine hesitancy has been rising, so much so that the WHO listed it as one of the top ten threats to world health in 2019.
Vaccine hesitancy is caused by mistrust, when people don’t trust vaccines’ safety or their effectiveness – or both.
According to the Wellcome Global Monitor – the world’s largest study into what people think and feel about science and health – globally only 79 per cent of people agree somewhat or strongly that vaccines are safe, with 7 per cent somewhat or strongly disagreeing. Another 11 per cent neither agree nor disagree, and 3 per cent don’t know.
The Global Monitor has shown that these levels of trust aren’t uniform across the world. People in high-income countries are less sure of vaccine safety. Only 72 per cent of people in Northern America and 73 per cent in Northern Europe agree that vaccines are safe. In Western Europe it’s is even lower, at 59 per cent, and in Eastern Europe it stands at only 40 per cent.
The opposite is true in low-income countries. The proportion of people who agree strongly or somewhat that vaccines are safe tends to sit at 80 per cent or above, with highs of 95 per cent in South Asia and 92 per cent in Eastern Africa.
We can’t say definitively what builds and erodes trust in vaccines. However, there is a correlation between trust and exposure to vaccine-preventable diseases. Where these diseases are endemic or their effects can be recently remembered, trust is higher. Conversely, where vaccines have removed the threat of disease and their effects aren’t immediately apparent, mistrust tends to appear.
Within regions, people who have high trust in doctors and nurses are consistently very likely to consider that vaccines are safe. Likewise, there is a clear positive relationship between overall trust in scientists and overall attitudes towards vaccines.
But there are also other, more complicated correlations – for example around education. In some places – like Northern Europe and Northern America – people with higher levels of science education are less likely to regard vaccines as unsafe. But in others – like Eastern Europe, Central Africa and Southern Africa – the opposite is true.
In certain places, we can hypothesise specific causes of mistrust. The long-debunked claims by Andrew Wakefield that the measles, mumps and rubella (MMR) vaccine was linked with autism are likely to be behind uptake of the vaccine falling in the UK.
And in Eastern Europe, where people are least likely to agree that vaccines are safe or effective, some researchers claim that vaccine scepticism may have been bolstered by Russian disinformation campaigns, which have amplified the vaccine debate on social media.
Did you find this content useful? Let us know your feedback at webmaster@wellcome.org.