10 Ways to Keep Breast Cancer Out of Your Future
Women have a 1 in 8 chance of developing breast cancer—here’s your step-by-step guide to preventing it.
The first time you purchased a bra, you likely had one of two thoughts about your breasts: you loved them, or you hated them. Your entire teenage life, your breasts constantly reminded you that you were a woman in training. You wanted them to grow bigger—and probably wished they’d stop growing at some point. Insecurities no doubt got to your head: Why is the left one bigger than the right one? Why aren’t they round like hers? Why are they getting so droopy?
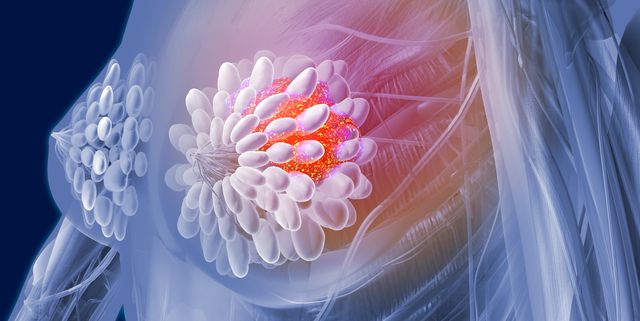
The truth is, no matter how conflicted you are about your breasts, they are part of your identity—which may be why, in part, having breast cancer is one of them most terrifying things to think about. Your breasts can say a lot about your health: they can signal weight gain, fluctuating hormones, and pregnancy.
As for lumps and bumps? You already know that can be a sign of something more sinister: breast cancer. Other than skin cancer, breast cancer is the most common cancer in U.S. women, with 1 in 8 women being affected by the disease, according to the American Cancer Society (ACS).
One bit of good news: fewer women are getting and dying from breast cancer than ever before. “Cancer is not an inevitability. Women have more control over the disease than they think,” says Margaret I. Cuomo, MD, author of A World Without Cancer. “Everything we do from the moment we wake—from what we eat and drink to whether or not we exercise and avoid BPA, parabens, and other carcinogenic chemicals—is a factor that can turn on or off the genetic switches in our bodies, including ones that could lead to cancer. The risk of many cancers, including breast cancer, can be significantly reduced by living a healthy lifestyle.”
Unfortunately, the biggest risk for breast cancer is simply being a woman—but taking certain measures can reduce your chances of developing the disease. Here’s where to start.

Dina Roth Port is a freelance writer for national magazines and the award-winning author of Previvors: Facing the Breast Cancer Gene and Making Life-Changing Decisions (Penguin, 2010). Her articles have appeared in Prevention, Glamour, Self, iVillage.com, The Huffington Post, Fitness, Cosmopolitan, Parenting, Parents, Martha Stewart Weddings and other titles. Roth Port lives in South Florida with her husband, two children, and two dogs. Check out her website at www.dinarothport.com.
Watch Next


Kate Middleton Diagnosed With Cancer at 42

Vitamin D and Calcium May Reduce Cancer Risk
How to Get the Right Team for Your Cancer Care
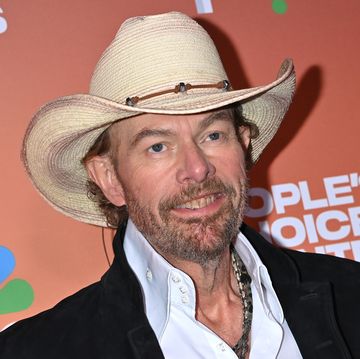
Toby Keith Dies at 62 After Stomach Cancer Battle