This story was originally published in 2015.
Story highlights
Fetal tissue has been used in biomedical research since the 1930s, including for the first polio vaccine
Cells from fetal tissue are still in use in vaccine manufacturing and stem cell and transplantation research
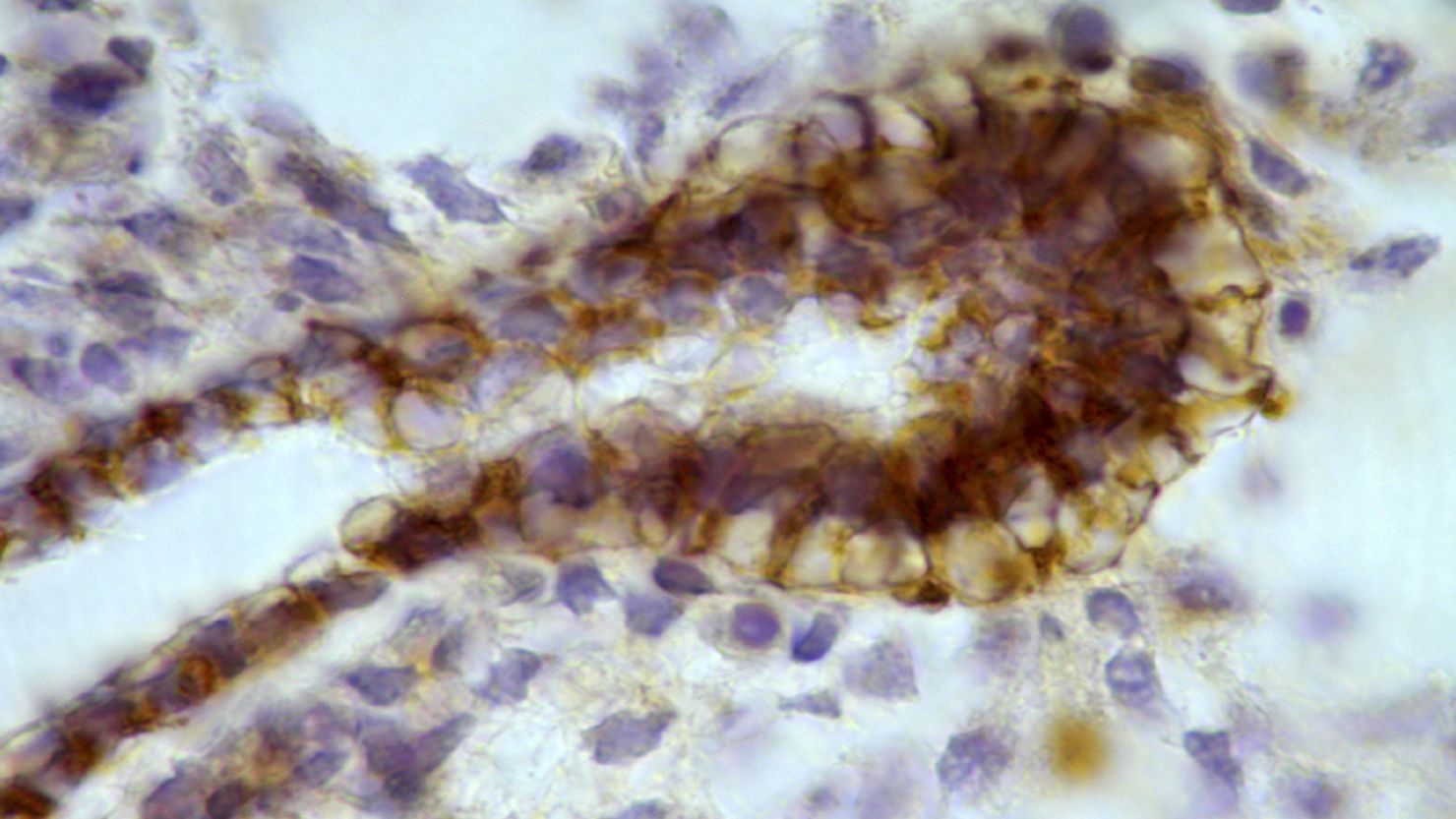
Fetal tissue has been used since the 1930s for vaccine development, and more recently to help advance stem cell research and treatments for degenerative diseases such as Parkinson’s disease. Researchers typically take tissue samples from a fetus that has been aborted (under conditions permitted by law) and grow cells from the tissue in Petri dishes.
Many of the uses of fetal tissue – and much of the debate – are not new. “It’s just that the public is finding out about it,” said Insoo Hyun, associate professor of bioethics at Case Western Reserve University.
In addition, the ways that fetal tissue are allowed to be obtained and used are not new either, Hyun said. The U.S. Department of Health and Human Services released guidelines on the topic in the 1990s.
The federal regulations state that women must decide to have an abortion before clinicians can ask whether they would like to donate fetal tissue. One concern is that women would have more pregnancies or abortions because they want to donate fetal tissue. In addition, clinicians performing the abortions cannot receive payment from researchers who will receive fetal materials, except for reimbursement for costs such as shipping.
Despite the long history of using fetal tissue in medicine and research, the practice could be on the way out. Even though it has led to important medical advances in the last several decades, “in the future, the need for fetal tissue will go down because of advances in stem cell [technology] that will take over,” Hyun said.
One of the earliest advances with fetal tissue was to use fetal kidney cells to create the first poliovirus vaccines, which are now estimated to save 550,000 lives worldwide every year.
In the early days of making the vaccine, researchers infected fetal kidney cells in Petri dishes to produce a large amount of virus that they could then harvest, purify and use to vaccinate people. (The virus evolves to become less deadly when it infects cells out of the body, and thus could safely be given to people to prime their immune system for the real thing.)
Today manufacturers of the polio vaccine use other types of human cells, which weren’t available in the mid-1900s. They also use monkey cells, which they originally avoided for fear that making the vaccine in animal cells could put people at risk of diseases from other species.
Many of our other common vaccines, such as chicken pox, rubella and shingles, have been produced in tissue derived from fetuses, particularly two electively terminated pregnancies from the 1960s. Advances in how researchers work with cells have allowed them to grow fetal cells indefinitely in Petri dishes, thus not requiring samples from any newly aborted fetuses.
Advances in stem cell therapy, too, could help phase out the practice of collecting cells from fetal tissue. Many researchers can now make stem cells by reprogramming skin cells from an adult into a “blank check” stem cell state. These so-called induced pluripotent stem cells can then go on to develop into neurons or any other cell in the body that researchers can grow in labs and study to better understand diseases such as Alzheimer’s disease.
However, as Hyun explained, research on these stem cells is still in the early stages and scientists need to make sure the neurons or whatever other type of cells they steer the stem cells to become behave like the cells in the body they want them to emulate. So scientists may still grow fetal neuron cells, for example, in a Petri dish alongside stem cell-derived neuron cells as a reference point until they have more confidence in the stem cell technology, said Hyun, who specifically studies the bioethics of stem cell research.
“The use of fetal tissue may also be supplanted in some cases by cells from umbilical cord blood. Amy Hudson, associate professor of microbiology and molecular genetics at Medical College of Wisconsin, has a grant from the National Institutes of Health to study how herpes viruses cause disease. Because it would be unethical to infect people and study disease in them, she and her colleagues plan to work with lab mice that have an altered immune system that behaves like that of humans. To achieve that, the researchers could transplant into the mice a small amount of liver tissue from fetuses: “a tiny number of cells that you can barely see,” Hudson said.
Yet just the practical challenges of doing this work, and especially the fact that the fetal tissue may not be available at the exact time they need them, are making Hudson and her colleagues think instead about using stem cells from the umbilical cord, which could be easier to obtain. However these cells do not appear to give mice as human-like an immune system. “The fear is we spend time and money on experiments using a halfway-OK [approach] and we get a result that isn’t interpretable,” Hudson said.
There are also a number of clinical research studies that are investigating whether transplanting different types of fetal tissue into patients could help them recover from diseases, similar to the practice of organ donation. One such study is testing fetal eye (retinal) tissue as a possible treatment for retinitis pigmentosa, a disease that can lead to blindness.
A lot of research in the last 10 years has also focused on using fetal neuronal cells for Parkinson’s and another degenerative disease called Huntington’s. Although early research on this approach for Parkinson’s patients was not encouraging, a small subset of patients do appear to benefit from it.
Join the conversation
Nevertheless, clinical research on tissue transplantation as a disease treatment may eventually be able to replace fetal tissue with stem cells, Hyun said. One of the Health and Human Services requirements for using fetal tissue is that no other experimental settings, such as other cell types or lab mice, would be appropriate.
When fetal tissue is used in research, it is often sent from the hospital or clinic that performs the abortion to an affiliated research center, Hyun said. Another safeguard in the Health and Human Services guidelines is that a clinical team that performs the abortion cannot know that the fetus will be donated, to help ensure that they do not change how they perform the abortion, or jeopardize the safety of the woman, Hyun said.
These guidelines have been solidified and become more widespread since the 1990s, Hyun said, adding that, “I believe [all clinicians] are well aware of them now.”