Prolonged or repeated respiratory tract illness is not inevitable for your athlete – do you just need to systematically assess respiratory health to help prevent it?
Respiratory tract illnesses (RTI) are the number one acute medical cause of time loss for athletes during major competitions and is an often-overlooked area of athlete care. RTI have traditionally been thought of as an unfortunate and unavoidable by-product of intense training, illness-inducing environments and hectic travel schedules(1). Over the last decade however, several studies have consistently demonstrated that respiratory issues are prevalent, often under-diagnosed, and not treated optimally in professional athletes, leaving them at higher risk of RTI susceptibility. We explore how a systematic approach to athlete respiratory health could help reduce the risk of illness and improve availability for performance.

What do we know about exercise-induced bronchoconstriction (EIB) & asthma in athletes?
Exercise-induced bronchoconstriction (EIB) is a condition that can negatively impact the health and performance of athletes yet is easily identified with objective (eucapnic voluntary hyperpnoea – EVH) testing and treatable with standard asthma medications depending on severity. A study by Jackson et al of 97 elite footballers found that 27 players had a positive test for EIB of which 38% had no documented history of asthma or EIB in the past (2). Of those players with a pre-existing history of EIB or asthma, 71% were under- or over-medicated, with some lacking objective evidence to support their pre-existing diagnosis (2).
Appropriate treatment was associated with a non-significant increase in maximal oxygen uptake and a significant improvement in spirometry values in a cohort of these elite level footballers who were followed up 9 weeks later. Under-diagnosis of EIB, and under-or over-medication, may pose a risk to the health of athletes, and have an impact on performance. The prevalence of this condition in this athletic cohort, and the poor relationship with symptoms, highlights the need for increased awareness and objective testing for EIB. This may also act as a blueprint for how to systematically investigate, diagnose and treat all respiratory conditions in athletes.
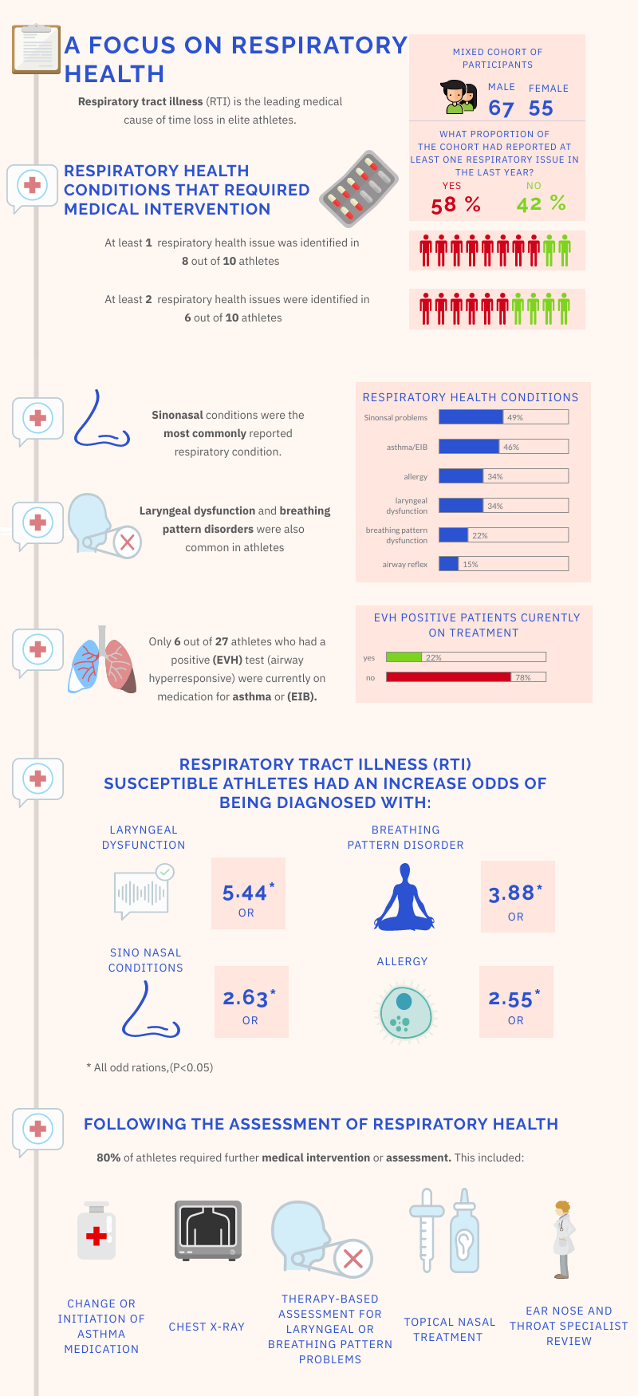
The (SARAH) project and associated study, is the first of its kind to systematically assess the respiratory health of elite athletes across twenty-four UK Olympic sports programmes(2). 122 Athletes, ¾ of whom were classified as ‘susceptible’ to respiratory illness, underwent a ‘total airway’ assessment that included a questionnaire, clinical interview, physiological investigations and allergy skin prick testing. Although previous studies have looked at identifying single respiratory health issues in isolation, this is the first study that has focused on the simultaneous prevalence and co-existence of multiple respiratory conditions, and how multiple components might impact respiratory function or illness susceptibility in athletes.
Following an initial assessment:
• At least 1 respiratory health issue was identified in 8 out of 10 athletes
• At least 2 respiratory health issues were identified in 6 out of 10 athletes
What was found? An interplay of risk factors
• Sino-nasal and asthma or EIB related conditions were common in athletes, with a trend of being underdiagnosed or not being treated optimally.
• Only 1 in 5 athletes with evidence of airway hyper responsiveness to exercise (positive EVH test) were receiving medical therapy for this.
• 1 in 3 athletes reported laryngeal dysfunction symptoms.
• RTI susceptibility increased the odds of being diagnosed with laryngeal dysfunction by over 5 times compared to non RTI susceptibility in athletes.
*Study limitation – As the study required athletes to be referred for assessment, patients with respiratory issues were over-represented.
What are the potential issues with poor adherence to medication, and the consequences of sub-optimal therapy?
• Poor adherence to medical therapy is associated with an increased risk of asthma exacerbations which could impact athlete’s availability and performance.
• Current adherence rates to medical therapy vary significantly (30-70%) in non-athlete adult populations (3) and elite athlete populations (4).
• Factors that impact adherence with medication therapy include patient knowledge, education, inhaler device convenience, age and adverse effects.
“Time loss from Respiratory Tract Illness (RTI) = exposure x respiratory susceptibility”
This study helps to support the concept that RTI is far from an “inevitable” and “unfortunate” consequence of high training loads in athletes. Athletes who have an underlying respiratory health condition were more likely to be susceptible to RTIs and suffer time loss from training. Although not directly assessed in the study, the high prevalence of undiagnosed respiratory conditions could suggest a link between respiratory illness risk and performance in athletes. Future prospective studies with randomised trials will be needed to investigate this further.
A systematic approach to the assessment, diagnosis and treatment of underlying respiratory conditions can help to reduce the risk of RTI, and this is an exciting area of research for sports clinicians. The SARAH study highlights how RTIs may not always be due to an infection or “infective pathogen” – but instead undiagnosed or over or under treated airway dysfunction or airway inflammation.
An expert panel at the IOC is currently looking at the issues of athlete respiratory health and will be issuing guidance on strategies and best practice guidance to reduce the burden on RTI in athletes in the future.
Take-Home Points:
• Respiratory conditions are common in elite athletes, with 4 out of 5 elite athletes in a group of mostly susceptible cohort reporting at least one respiratory condition that required further evaluation (EIS SARAH study).
• Respiratory tract illness (RTI) susceptibility is associated with an increased odds ratio of underlying respiratory issues.
• Exclusively symptom-based diagnosis of respiratory conditions can lead to under or over diagnosis if not combined with objective testing.
Authors and Affiliations:
Hassan Khan, David Whittaker, Sidra Awan, Aessa Tumi, Katija Ali, Kosta Ikonomou, Irfan Ahmed.
1. Mr Hassan Khan is a 5th year medical student at University College London.
Email: zchah02@ucl.ac.uk Twitter: @hass_khan
2. Dr David Whittaker is a Sport and Exercise Medicine Registrar based in London (UK). He has an interest in injury prevention, exercise testing and the use of physical activity to prevent and manage chronic disease.
3. Dr Aessa Tumi is a GP Trainee on the St Mary’s VTS, London. He has an interest in musculoskeletal, sport and exercise medicine.
4. Ms Sidra A.Awan is a Senior Critical Care Pharmacist and National Institute for Health Research ICA Intern. She has an interest in intensive care medicine and is currently working at University College London Hospital.
5. Dr Katija Ali is a General Practitioner based in London (UK) with a special interest in exercise prescription in chronic disease management and primary care musculoskeletal problems.
Twitter @KatijaAli
6. Kosta Ikonomou is a sports physiotherapist based in Vancouver, Canada. His professional and academic expertise lies in musculoskeletal injuries, concussion, and exercise based therapies for injury prevention and elite performance.
Twitter: @thesmileyphysio
7. Dr Irfan Ahmed is a Sport & Exercise Medicine Registrar and General Practitioner based in London (UK). He has an interest in VO2 max, injury prevention and also using exercise to help prevent chronic disease and rehabilitate patients.
Twitter @Exerciseirfan
References:
1. Levai I, Hull J, Loosemore M, Greenwell J, Whyte G, Dickinson J. Environmental influence on the prevalence and pattern of airway dysfunction in elite athletes. Respirology. 2016;21(8):1391-1396.
2. Hull J, Jackson A, Ranson C, Brown F, Wootten M, Loosemore M. The benefits of a systematic assessment of respiratory health in illness susceptible athletes. European Respiratory Journal. 2020;:2003722.
3. Engelkes M, Janssens H, de Jongste J, Sturkenboom M, Verhamme K. Medication adherence and the risk of severe asthma exacerbations: a systematic review. European Respiratory Journal. 2014;45(2):396-407.
4. Jackson A, Hull J, Hopker J, Dickinson J. Impact of detecting and treating exercise-induced bronchoconstriction in elite footballers. ERJ Open Research. 2018;4(2):00122-2017.
No conflicts of interests to declare.
Acknowledgements – We would like to acknowledge the support of authors of the SARAH study for review of this blog. Twitter : @TheISEH