Intravascular healing is not affected by approaches in contemporary CTO PCI: the CONSISTENT CTO study
Selected in JACC Cardiovascular Interventions by N. Ryan
This study compares clinical, angiographic and imaging outcomes of patients undergoing CTO PCI with dissection and re-entry techniques (DART) and subintimal stenting to intimal techniques.
References
Authors
Walsh SJ, Hanratty CG, McEntegart M, Strange JW, Rigger J, Henriksen PA, Smith EJ, Wilson SJ, Hill JM, Mehmedbegovic Z, Chevalier B, Morice MC and Spratt JC
Reference
JACC Cardiovascular Interventions. Volume 13, Issue 12, June 2020. DOI: 10.1016/j.jcin.2020.03.032
Published
June 2020
Link
Read the abstractReviewer
Latest contributions
Comparison of two self-expanding transcatheter heart valves for degenerated surgical bioprostheses: the AVENGER multicentre registry Long-term beta-blocker treatment after acute myocardial infarction and preserved left ventricular ejection fraction: The REDUCE-AMI Trial Coronary vasomotor dysfunction is associated with cardiovascular events in patients with nonobstructive coronary artery diseaseMy Comment
Why this study? – the rationale/objective
The CONSISTENT CTO study was a single-arm prospective multicentre trial comparing clinical, angiographic and imaging outcomes of patients undergoing CTO PCI with dissection and re-entry techniques (DART) and subintimal stenting, to intimal techniques and stenting, using an everolimus eluting stent with a bioabsorbable polymer.
CTO PCI is a challenging subset of PCI with DART commonly required for more complex CTO’s. There is limited data regarding the longer-term outcomes of DART with concerns raised with regard to poorer outcomes with potentially adverse intravascular healing. Furthermore, previous IVUS studies have shown discrepancies between the operators presumed and actual mode of CTO crossing, therefore, raising doubts with regard to the applicability of previous comparisons of DART and intimal crossing in current practice.
How was it executed? – the methodology
Patients undergoing clinically indicated (mainly stable angina, 83.3%) CTO PCI were consented and completed baseline quality of life assessments (231) once the CTO was successfully crossed the patients were included in the trial (210) – success rate 91%. Planned angiography/lesion optimisation within 12 weeks of the index procedure was allowed per protocol.
- PCI technique was at the discretion of the operator and a pre-stenting IVUS was mandated to determine if the wire tracking was intimal or subintimal.
- Patients underwent clinical and angiographic follow up with OCT at 12 months and clinical follow up at 24 months.
- The primary device-related endpoint was target vessel failure (TVF) at 12 months – a composite of cardiac death, MI related to the target vessel or ischemia driven TVR.
- The majority of the patients were male (81.4%) with a mean age of 63.5±10.7 years. Slightly more than half (51.4%) had LV impairment, with 1.9% severe LV impairment.
What is the main result?
The operator presumed final successful strategy was AWE in 72 (34.3%), RWE in 37 (17.6%), ADR in 38 (18.1%) and RDR in 63 (30%). Three patients withdrew consent with clinical, angiographic and OCT follow up available in 206/207 (99.5%), 188 (90.8%) and 175 (94.5%) patients respectively at 12 months and clinical follow up in 99.5% at 24 months.
- Pre-stent IVUS was available in 190 (90.5%) with discordance between the actual and presumed wire pathway in 15.8% of cases.
- Patients treated with DART had more complex (J-CTO score 2.9±1.2 vs. 2.0±1.1, p<0.001) and longer lesions (lesion length 36.3±22.0mm vs. 22.6±16.6mm, p <0.0001, stent length 96.6±±31.6mm vs. 75.4±31.4mm, p<0.0001) and more commonly had a prior CABG to the CTO vessel (21.8% vs. 10.1%, p=0.023).
- TVF occurred in 12/210 (5.7%) at 12 months with a TVF rate of 10% at 24 months. Using multivariate analysis there was no significant association between TVF and strategy at 12 months (p=0.893).
- MACE (all-cause mortality, MI, TVR) was 10% at 12 months and 17% at 24 months. There was a 7.1% rate of TVR at 12 months and 11.9% at 24 months.
- Comparing DART to no-DART MACE was numerically but not statistically higher at 12 months (13.9% vs. 6.4%, p=0.073) and 24 months (14.9% vs. 9.2%, p=0.177). TVR rates at 12 months and 24 months were 10.9% vs. 3.7%, p=0.042 and 14.9% vs. 9.2% p=0.204 respectively.
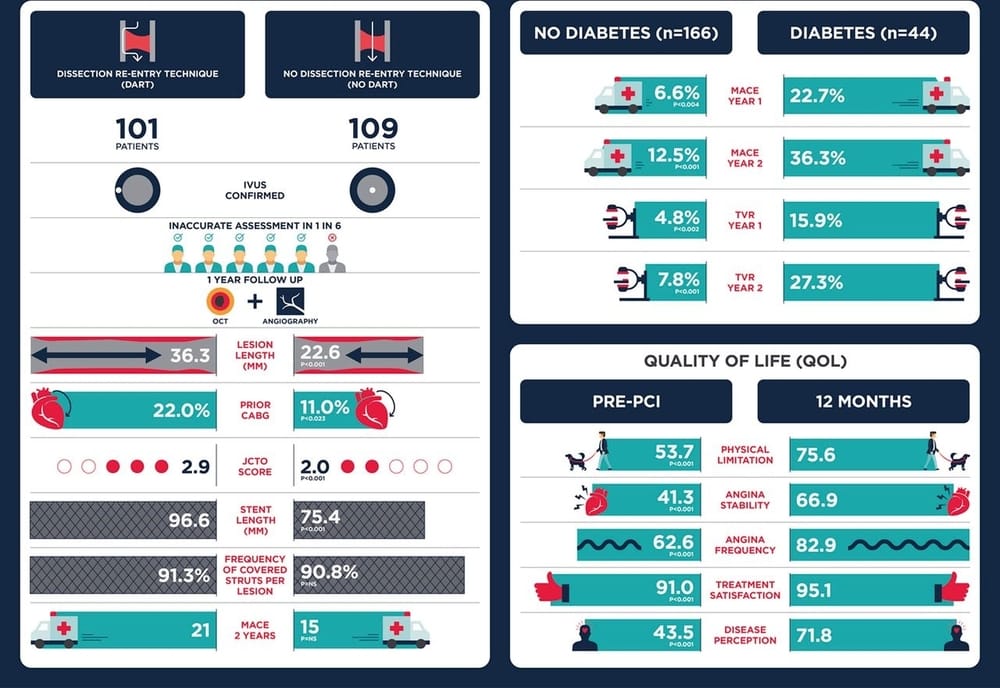
- In patients with diabetes MACE and TVR were significantly higher at both 12 and 24 months (MACE 22.7% vs 6.6%, p=0.004, 36.3% vs. 12.5% p=0.0001, TVR 15.9% vs. 4.8%, p=0.02, 27.3% vs.7.8%, p=0.004 at 12 and 24 months respectively).
- Full OCT analysis was available in 167 with no difference in strut coverage (DART vs. no DART 90.1±10.0 vs. 91.9±9.6, p=0.238) or malapposed struts (DART vs. no-DART, 2.9±4.7 vs. 2.2±4.6, p=0.334).
- There was significant improvement in all components of the SAQ at 12 months.
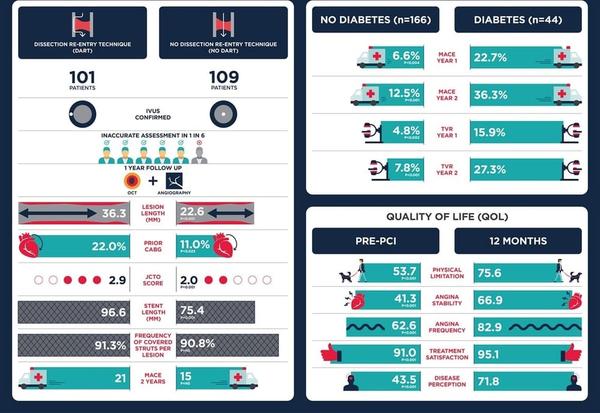
Illustration credit: JACC Cardiovascular Interventions
Critical reading and the relevance for clinical practice
The results of this trial show that contemporary CTO techniques have a high initial success rate with durable short and medium-term clinical outcomes irrespective of the technique used. The overall rates of both TVF and MACE are low and in keeping with trials in complex non-CTO PCI. Similar to previous studies there are discrepancies in operator perceived and actual wire pathway in approximately 15% of cases, however, OCT analysis confirmed no differences in strut coverage or malapposition by technique. As with prior PCI trials, the presence of diabetes had a significant impact with poorer outcomes at both 12 and 24 months.
A note of caution when interpreting the results, one must bear in mind that all operators in this trial were experienced CTO PCI operators and these outcomes may not be generalisable. There was a significant improvement in quality of life with the enrolled patients self-reporting severe limitations prior to the procedure, however, there was no medical therapy or sham procedure control arm.
In appropriately selected patients, experienced operators can achieve good clinical and angiographic outcomes with significant improvements in patients' quality of life. Further trials looking at longer term durability and intravascular healing will further add to our knowledge basis in this group. Randomised control trials comparing PCI with sham procedures and medical management would be of interest. However, as demonstrated in DECISION-CTO and EURO-CTO, it may be difficult to recruit the most symptomatic patients to these trials.




No comments yet!