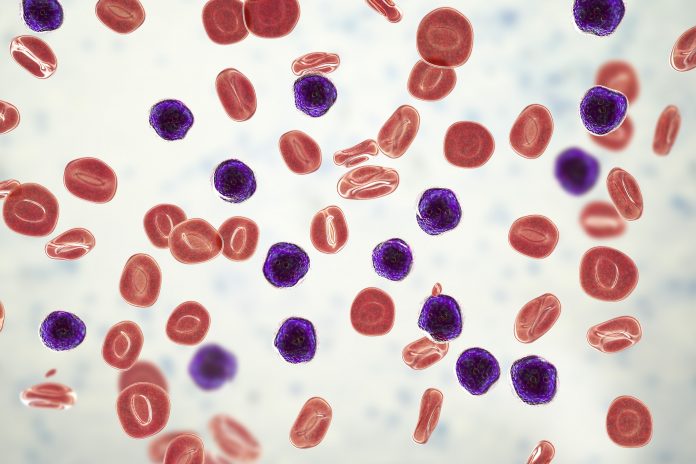
In pediatric and young adult patients with acute lymphoblastic leukemia (ALL) treated with tisagenlecleucel (Kymriah), DNA sequencing-based detection of residual disease identified all patients who would eventually relapse, and was more accurate than flow cytometry.
While flow cytometry could detect approximately one cancer cell per 10,000 blood cells, NGS-MRD was far more sensitive, with the ability to detect one cancer cell per 1 to 10 million blood cells, depending on the number of cells in the sample. This resulted in 131 percent more positive samples detected via NGS-MRD compared with flow cytometry.
The study was published today in Blood Cancer Discovery. The lead author was Michael Pulsipher, M.D., a professor of pediatrics and the division chief of Pediatric Hematology and Oncology at Intermountain Primary Children’s Hospital and the Huntsman Cancer Institute of the University of Utah.
Tisagenlecleucel is a chimeric antigen receptor T-cell (CAR-T) treatment and Pulsipher said that more than 80% of ALL patients treated this way experience a complete remission. However, around half of patients eventually relapse and require additional treatment, such as a bone marrow transplant. Accurately predicting relapse could allow patients who need a transplant to begin the process before the disease actually recurs.
“Our current recommendation to centers giving tisagenlecleucel is to follow B cells in the blood monthly, using a standard test, as a way to predict patients at higher risk of relapse,” said Stephan Grupp, M.D., Ph.D., senior author of the study and a professor of pediatrics and the chief of Cell Therapy and Transplant at Children’s Hospital of Philadelphia and the University of Pennsylvania. However, “Monitoring B-cell aplasia is not ideal because it only picks up part of the relapse risk,” Grupp said.
Liquid biopsies that investigate markers in the blood or bone marrow have increased in popularity, but these methods have not been directly compared. In this study, Pulsipher and colleagues investigated the predictive value of flow cytometry and next-generation DNA sequencing minimal residual disease (NGS-MRD) monitoring, using blood and bone marrow samples collected from the ELIANA and ENSIGN phase II clinical trials at one, three, six, nine, and 12 months after tisagenlecleucel infusion.
For flow cytometry, cells were analyzed for the presence of CD9, CD10, CD13, CD19, CD20, CD22, CD33, CD34, CD38, CD45, CD58, CD66c, and CD123. For NGS, the gene sequences of IgH, IgK, and IgL were analyzed for rearrangements and translocations.
NGS-MRD of bone marrow samples was more accurate in predicting relapse than flow cytometry. Of patients with any detectable disease DNA at three- or six-months post-infusion, 100% experienced either a relapse or progression to another therapy, with the exception of one patient lost to follow-up. NGS-MRD detection was also able to find those at risk well in advance of relapse. Those who had NGS-MRD positivity at the lowest levels relapsed a median of 168 days after the positive test, and the assay detected 100 percent of the relapses. By contrast, flow cytometry was positive at a median 52 days prior to relapse and missed 50 percent of the relapses.
These data suggest that the more sensitive NGS measurements detect disease with sufficient lead time prior to relapse to allow repeat sampling and/or coordination of therapeutic interventions, Pulsipher said.
“This is the first paper to show an approach that identifies markers of relapse that are very specific, allowing clinicians to add additional therapy prior to relapse that will prevent it,” Pulsipher said.