Abstract
Purpose
Clinical research studies over the last 15 years have reported a significant burden of hypopituitarism in survivors of traumatic brain injury (TBI). However, debate still exists about the true prevalence of hypopituitarism after head injury.
Methods
We have reviewed the literature describing the frequency of post-traumatic hypopituitarism and discuss the factors which may explain the variable frequency of the reported deficits in clinical studies including research methodology and the natural history of the disease.
Results
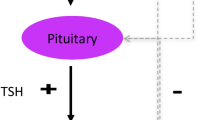
Pituitary hormone perturbations in the acute phase following injury are frequent but are difficult to attribute to traumatic pituitary damage due to physiological hormonal changes in acute illness, the confounding effect of medications, other co-morbidities and lack of appropriate control subjects. Nevertheless, a small number of studies have emphasised the clinical importance of acute, dynamic disturbance of the hypothalamic–pituitary–adrenal axis. There is a much larger evidence base examining the frequency of hypopituitarism in the chronic, recovery phase following head injury. These studies report a very broad prevalence of long-term pituitary hormone dysfunction in survivors of TBI. However, systematic review suggests the prevalence to be between 27 and 31%.
Conclusion
Survivors of head injury are at risk of pituitary hormone dysfunction and we suggest an approach to the diagnosis of post-traumatic hypopituitarism in routine clinical practice.

Reproduced with permission from [10]

Similar content being viewed by others
References
Langlois JA, Rutland-Brown W, Wald MM (2006) The epidemiology and impact of traumatic brain injury: a brief overview. J Head Trauma Rehabil 21(5):375–378
Tagliaferri F, Compagnone C, Korsic M, Servadei F, Kraus J (2006) A systematic review of brain injury epidemiology in Europe. Acta Neurochir (Wien) 148(3):255–268. https://doi.org/10.1007/s00701-005-0651-y; discussion 268.
Taylor CA, Bell JM, Breiding MJ, Xu L (2017) Traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ 66(9):1–16. https://doi.org/10.15585/mmwr.ss6609a1
Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE (1999) Traumatic brain injury in the United States: a public health perspective. J Head Trauma Rehabil 14(6):602–615
Cyran E (1918) Hypophysenschädigung durch schädelbasisfraktur. Dtsch Med Wochenschr 44(45):1261
Harper CG, Doyle D, Adams JH, Graham DI (1986) Analysis of abnormalities in pituitary gland in non-missile head injury: study of 100 consecutive cases. J Clin Pathol 39(7):769–773
Kibayashi K, Shimada R, Nakao K, Ro A (2012) Analysis of pituitary lesions in fatal closed head injury. Am J Forensic Med Pathol 33(3):206–210. https://doi.org/10.1097/PAF.0b013e3181fe33e8
Schneider HJ, Kreitschmann-Andermahr I, Ghigo E, Stalla GK, Agha A (2007) Hypothalamopituitary dysfunction following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a systematic review. JAMA 298(12):1429–1438. https://doi.org/10.1001/jama.298.12.1429
Tanriverdi F, Unluhizarci K, Kelestimur F (2010) Pituitary function in subjects with mild traumatic brain injury: a review of literature and proposal of a screening strategy. Pituitary 13(2):146–153. https://doi.org/10.1007/s11102-009-0215-x
Agha A, Phillips J, O’Kelly P, Tormey W, Thompson CJ (2005) The natural history of post-traumatic hypopituitarism: implications for assessment and treatment. Am J Med 118(12):1416. https://doi.org/10.1016/j.amjmed.2005.02.042
Klose M, Juul A, Struck J, Morgenthaler NG, Kosteljanetz M, Feldt-Rasmussen U (2007) Acute and long-term pituitary insufficiency in traumatic brain injury: a prospective single-centre study. Clin Endocrinol (Oxf) 67(4):598–606. https://doi.org/10.1111/j.1365-2265.2007.02931.x
Tanriverdi F, De Bellis A, Ulutabanca H, Bizzarro A, Sinisi AA, Bellastella G, Paglionico A, Dalla Mora V, Selcuklu L, Unluhizarci A, Casanueva K, Kelestimur FF (2013) F.: A five year prospective investigation of anterior pituitary function after traumatic brain injury: is hypopituitarism long-term after head trauma associated with autoimmunity? J Neurotrauma 30(16):1426–1433. https://doi.org/10.1089/neu.2012.2752
Klose M, Stochholm K, Janukonyte J, Lehman Christensen L, Frystyk J, Andersen M, Laurberg P, Christiansen JS, Feldt-Rasmussen U (2014) Prevalence of posttraumatic growth hormone deficiency is highly dependent on the diagnostic set-up: results from The Danish National Study on Posttraumatic Hypopituitarism. J Clin Endocrinol Metab 99(1):101–110. https://doi.org/10.1210/jc.2013-2397
Agha A, Rogers B, Sherlock M, O’Kelly P, Tormey W, Phillips J, Thompson CJ (2004) Anterior pituitary dysfunction in survivors of traumatic brain injury. J Clin Endocrinol Metab 89(10):4929–4936. https://doi.org/10.1210/jc.2004-0511
Kokshoorn NE, Smit JW, Nieuwlaat WA, Tiemensma J, Bisschop PH, Veldman G, Roelfsema R, Franken F, Wassenaar AA, Biermasz MJ, Romijn NR, Pereira JA (2011) A.M.: Low prevalence of hypopituitarism after traumatic brain injury: a multicenter study. Eur J Endocrinol 165(2):225–231. https://doi.org/10.1530/EJE-11-0365
Tanriverdi F, Senyurek H, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2006) High risk of hypopituitarism after traumatic brain injury: a prospective investigation of anterior pituitary function in the acute phase and 12 months after trauma. J Clin Endocrinol Metab 91(6):2105–2111. https://doi.org/10.1210/jc.2005-2476
Agha A, Rogers B, Mylotte D, Taleb F, Tormey W, Phillips J, Thompson CJ (2004) Neuroendocrine dysfunction in the acute phase of traumatic brain injury. Clin Endocrinol (Oxf) 60(5):584–591. https://doi.org/10.1111/j.1365-2265.2004.02023.x
Hannon MJ, Crowley RK, Behan LA, O’Sullivan EP, O’Brien MM, Sherlock M, Rawluk D, O’Dwyer R, Tormey W, Thompson CJ (2013) Acute glucocorticoid deficiency and diabetes insipidus are common after acute traumatic brain injury and predict mortality. J Clin Endocrinol Metab 98(8):3229–3237. https://doi.org/10.1210/jc.2013-1555
Cohan P, Wang C, McArthur DL, Cook SW, Dusick JR, Armin B, Swerdloff R, Vespa P, Muizelaar JP, Cryer HG, Christenson PD, Kelly DF (2005) Acute secondary adrenal insufficiency after traumatic brain injury: a prospective study. Crit Care Med 33(10):2358–2366
Hackl JM, Gottardis M, Wieser CH, Rumpl E, Stadler C, Schwarz S, Monkayo R (1991) Endocrine abnormalities in severe traumatic brain injury—a cue to prognosis in severe craniocerebral trauma? Intensive Care Med 17(1):25–29
Cernak I, Savic VJ, Lazarov A, Joksimovic M, Markovic S (1999) Neuroendocrine responses following graded traumatic brain injury in male adults. Brain injury 13(12):1005–1015
Alavi SA, Tan CL, Menon DK, Simpson HL, Hutchinson PJ (2016) Incidence of pituitary dysfunction following traumatic brain injury: A prospective study from a regional neurosurgical centre. Br J Neurosurg 30(3):302–306. https://doi.org/10.3109/02688697.2015.1109060
Bensalah M, Donaldson M, Aribi Y, Iabassen M, Cherfi L, Nebbal M, Medjaher M, Haffaf E, Abdennebi B, Guenane K, Djermane A, Kemali Z, OuldKablia S (2018) Cortisol evaluation during the acute phase of traumatic brain injury-A prospective study. Clin Endocrinol (Oxf) 88(5):627–636. https://doi.org/10.1111/cen.13562
Tanriverdi F, Ulutabanca H, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2008) Three years prospective investigation of anterior pituitary function after traumatic brain injury: a pilot study. Clin Endocrinol (Oxf) 68(4):573–579. https://doi.org/10.1111/j.1365-2265.2007.03070.x
Kokshoorn NE, Wassenaar MJ, Biermasz NR, Roelfsema F, Smit JW, Romijn JA, Pereira AM (2010) Hypopituitarism following traumatic brain injury: prevalence is affected by the use of different dynamic tests and different normal values. Eur J Endocrinol 162(1):11–18. https://doi.org/10.1530/EJE-09-0601
Klose M, Juul A, Poulsgaard L, Kosteljanetz M, Brennum J, Feldt-Rasmussen U (2007) Prevalence and predictive factors of post-traumatic hypopituitarism. Clin Endocrinol (Oxf) 67(2):193–201. https://doi.org/10.1111/j.1365-2265.2007.02860.x
Kelly DF, Gaw Gonzalo IT, Cohan P, Berman N, Swerdloff R, Wang C (2000) Hypopituitarism following traumatic brain injury and aneurysmal subarachnoid hemorrhage: a preliminary report. J Neurosurg 93(5):743–752. https://doi.org/10.3171/jns.2000.93.5.0743
Bondanelli M, De Marinis L, Ambrosio MR, Monesi M, Valle D, Zatelli MC, Fusco A, Bianchi A, Farneti M, Degli ECI (2004) Occurrence of pituitary dysfunction following traumatic brain injury. J Neurotrauma 21(6):685–696
Bavisetty S, McArthur DL, Dusick JR, Wang C, Cohan P, Boscardin WJ, Swerdloff R, Levin H, Chang DJ, Muizelaar JP, Kelly DF (2008) Chronic hypopituitarism after traumatic brain injury: risk assessment and relationship to outcome. Neurosurgery 62(5):1080–1093. https://doi.org/10.1227/01.neu.0000325870.60129.6a discussion 1093 – 1084
Silva PP, Bhatnagar S, Herman SD, Zafonte R, Klibanski A, Miller KK, Tritos NA (2015) Predictors of hypopituitarism in patients with traumatic brain injury. J Neurotrauma 32(22):1789–1795. https://doi.org/10.1089/neu.2015.3998
Schneider M, Schneider HJ, Yassouridis A, Saller B, von Rosen F, Stalla GK (2008) Predictors of anterior pituitary insufficiency after traumatic brain injury. Clin Endocrinol (Oxf) 68(2):206–212. https://doi.org/10.1111/j.1365-2265.2007.03020.x
Zheng P, He B, Guo Y, Zeng J, Tong W (2015) Decreased apparent diffusion coefficient in the pituitary and correlation with hypopituitarism in patients with traumatic brain injury. J Neurosurg 123(1):75–80. https://doi.org/10.3171/2014.12.JNS132308
Tanriverdi F, Schneider HJ, Aimaretti G, Masel BE, Casanueva FF, Kelestimur F (2015) Pituitary dysfunction after traumatic brain injury: a clinical and pathophysiological approach. Endocr Rev 36(3):305–342. https://doi.org/10.1210/er.2014-1065
Aimaretti G, Ambrosio MR, Di Somma C, Gasperi M, Cannavo S, Scaroni C, Fusco A, Del Monte P, De Menis E, Faustini-Fustini M, Grimaldi F, Logoluso F, Razzore P, Rovere S, Benvenga S, Uberti D, De Marinis EC, Lombardi L, Mantero G, Martino F, Giordano E, Ghigo G (2005) E.: Residual pituitary function after brain injury-induced hypopituitarism: a prospective 12-month study. J Clin Endocrinol Metab 90(11):6085–6092. https://doi.org/10.1210/jc.2005-0504
Schneider HJ, Schneider M, Saller B, Petersenn S, Uhr M, Husemann B, von Rosen F, Stalla GK (2006) Prevalence of anterior pituitary insufficiency 3 and 12 months after traumatic brain injury. Eur J Endocrinol 154(2):259–265. https://doi.org/10.1530/eje.1.02071
Lauzier F, Turgeon AF, Boutin A, Shemilt M, Côté I, Lachance O, Archambault PM, Lamontagne F, Moore L, Bernard F, Gagnon C, Cook D (2014) Clinical outcomes, predictors, and prevalence of anterior pituitary disorders following traumatic brain injury: a systematic review. Crit Care Med 42(3):712–721. https://doi.org/10.1097/CCM.0000000000000046
Agha A, Thornton E, O’Kelly P, Tormey W, Phillips J, Thompson CJ (2004) Posterior pituitary dysfunction after traumatic brain injury. J Clin Endocrinol Metab 89(12):5987–5992. https://doi.org/10.1210/jc.2004-1058
Hadjizacharia P, Beale EO, Inaba K, Chan LS, Demetriades D (2008) Acute diabetes insipidus in severe head injury: a prospective study. J Am Coll Surg 207(4):477–484. https://doi.org/10.1016/j.jamcollsurg.2008.04.017
Benvenga S, Campenni A, Ruggeri RM, Trimarchi F (2000) Clinical review 113: hypopituitarism secondary to head trauma. J Clin Endocrinol Metab 85(4):1353–1361. https://doi.org/10.1210/jcem.85.4.6506
Karali V, Massa E, Vassiliadou G, Chouris I, Rodin I, Bitzani M (2008) Evaluation of development of diabetes insipidus in the early phase following traumatic brain injury in critically ill patients. Crit Care 12(2):P130. https://doi.org/10.1186/cc6351
Boughey JC, Yost MJ, Bynoe RP (2004) Diabetes insipidus in the head-injured patient. Am Surg 70(6):500–503
Wong MF, Chin NM, Lew TW (1998) Diabetes insipidus in neurosurgical patients. Ann Acad Med Singapore 27(3):340–343
Maggiore U, Picetti E, Antonucci E, Parenti E, Regolisti G, Mergoni M, Vezzani A, Cabassi A, Fiaccadori E (2009) The relation between the incidence of hypernatremia and mortality in patients with severe traumatic brain injury. Crit Care 13(4):R110
Tanriverdi F, Unluhizarci K, Kocyigit I, Tuna IS, Karaca Z, Durak AC, Selcuklu A, Casanueva FF, Kelestimur F (2008) Brief communication: pituitary volume and function in competing and retired male boxers. Ann Intern Med 148(11):827–831
Tanriverdi F, Unluhizarci K, Coksevim B, Selcuklu A, Casanueva FF, Kelestimur F (2007) Kickboxing sport as a new cause of traumatic brain injury-mediated hypopituitarism. Clin Endocrinol (Oxf) 66(3):360–366. https://doi.org/10.1111/j.1365-2265.2006.02737.x
Kelly DF, Chaloner C, Evans D, Mathews A, Cohan P, Wang C, Swerdloff R, Sim MS, Lee J, Wright MJ, Kernan C, Barkhoudarian G, Yuen KC, Guskiewicz K (2014) Prevalence of pituitary hormone dysfunction, metabolic syndrome, and impaired quality of life in retired professional football players: a prospective study. J Neurotrauma 31(13):1161–1171. https://doi.org/10.1089/neu.2013.3212
Wilkinson CW, Pagulayan KF, Petrie EC, Mayer CL, Colasurdo EA, Shofer JB, Hart KL, Hoff D, Tarabochia MA, Peskind ER (2012) High prevalence of chronic pituitary and target-organ hormone abnormalities after blast-related mild traumatic brain injury. Front Neurol 3:11. https://doi.org/10.3389/fneur.2012.00011
Tanriverdi F, Unluhizarci K, Karaca Z, Casanueva FF, Kelestimur F (2010) Hypopituitarism due to sports related head trauma and the effects of growth hormone replacement in retired amateur boxers. Pituitary 13(2):111–114. https://doi.org/10.1007/s11102-009-0204-0
Tanriverdi F, Unluhizarci K, Selcuklu A, Casanueva FF, Kelestimur F (2007) Transient hypogonadotropic hypogonadism in an amateur kickboxer after head trauma. J Endocrinol Invest 30(2):150–152
Undurti A, Colasurdo EA, Sikkema CL, Schultz JS, Peskind ER, Pagulayan KF, Wilkinson CW (2018) Chronic hypopituitarism associated with increased postconcussive symptoms is prevalent after blast-induced mild traumatic brain injury. Front Neurol 9:72. https://doi.org/10.3389/fneur.2018.00072
Baxter D, Sharp DJ, Feeney C, Papadopoulou D, Ham TE, Jilka S, Hellyer PJ, Patel MC, Bennett AN, Mistlin A, McGilloway E, Midwinter M, Goldstone AP (2013) Pituitary dysfunction after blast traumatic brain injury: The UK BIOSAP study. Ann Neurol 74(4):527–536. https://doi.org/10.1002/ana.23958
Foley CM, Wang DH (2012) Central diabetes insipidus following a sports-related concussion: a case report. Sports Health 4(2):139–141. https://doi.org/10.1177/1941738111434275
Zhou Y (2017) Abnormal structural and functional hypothalamic connectivity in mild traumatic brain injury. J Magn Reson Imaging 45(4):1105–1112. https://doi.org/10.1002/jmri.25413
Kelly P, Farrant B (2008) Shaken baby syndrome in New Zealand, 2000–2002. J Paediatr Child Health 44(3):99–107. https://doi.org/10.1111/j.1440-1754.2007.01234.x
Corrigan JD, Selassie AW, Orman JA (2010) The epidemiology of traumatic brain injury. J Head Trauma Rehabil 25(2):72–80. https://doi.org/10.1097/HTR.0b013e3181ccc8b4
Heather NL, Jefferies C, Hofman PL, Derraik JG, Brennan C, Kelly P, Hamill JK, Jones RG, Rowe DL, Cutfield WS (2012) Permanent hypopituitarism is rare after structural traumatic brain injury in early childhood. J Clin Endocrinol Metab 97(2):599–604. https://doi.org/10.1210/jc.2011-2284
Casano-Sancho P, Suárez L, Ibáñez L, García-Fructuoso G, Medina J, Febrer A (2013) Pituitary dysfunction after traumatic brain injury in children: is there a need for ongoing endocrine assessment? Clin Endocrinol (Oxf) 79(6):853–858. https://doi.org/10.1111/cen.12237
Bellone S, Einaudi S, Caputo M, Prodam F, Busti A, Belcastro S, Parlamento S, Zavattaro M, Verna F, Bondone C, Tessaris D, Gasco V, Bona G, Aimaretti G (2013) Measurement of height velocity is an useful marker for monitoring pituitary function in patients who had traumatic brain injury. Pituitary 16(4):499–506. https://doi.org/10.1007/s11102-012-0446-0
Einaudi S, Matarazzo P, Peretta P, Grossetti R, Giordano F, Altare F, Bondone C, Andreo M, Ivani G, Genitori L, de Sanctis C (2006) Hypothalamo-hypophysial dysfunction after traumatic brain injury in children and adolescents: a preliminary retrospective and prospective study. J Pediatr Endocrinol Metab 19(5):691–703
Personnier C, Crosnier H, Meyer P, Chevignard M, Flechtner I, Boddaert N, Breton S, Mignot C, Dassa Y, Souberbielle JC, Piketty M, Laborde K, Jais JP, Viaud M, Puget S, Sainte-Rose C, Polak M (2014) Prevalence of pituitary dysfunction after severe traumatic brain injury in children and adolescents: a large prospective study. J Clin Endocrinol Metab 99(6):2052–2060. https://doi.org/10.1210/jc.2013-4129
Kaulfers AM, Backeljauw PF, Reifschneider K, Blum S, Michaud L, Weiss M, Rose SR (2010) Endocrine dysfunction following traumatic brain injury in children. J Pediatr 157(6):894–899. https://doi.org/10.1016/j.jpeds.2010.07.004
Casano-Sancho P (2017) Pituitary dysfunction after traumatic brain injury: are there definitive data in children? Arch Dis Child 102(6):572
Agha A, Sherlock M, Thompson CJ (2005) Post-traumatic hyponatraemia due to acute hypopituitarism. QJM 98(6):463–464. https://doi.org/10.1093/qjmed/hci075
Hannon MJ, Behan CR, O’Sullivan LA, Rogers EP, O’Brien B, Rawluk MC, O’Dwyer D, Agha R, Thompson C (2011) Low total cortisol correlates closely with low free cortisol in traumatic brain injury and predicts mortality and long-term hypopituitarism. Endocr Rev 32(03):R28–24 Meeting Abstracts O
Tritos NA, Yuen KC, Kelly DF, Committee ANaPS: American Association of Clinical Endocrinologists and American College of Endocrinology Disease State Clinical Review (2015) A neuroendocrine approach to patients with traumatic brain injury. Endocr Pract 21(7), 823–831. https://doi.org/10.4158/EP14567.DSCR
Tan CL, Alavi SA, Baldeweg SE, Belli A, Carson A, Feeney C, Goldstone AP, Greenwood R, Menon DK, Simpson HL, Toogood AA, Gurnell M, Hutchinson PJ (2017) The screening and management of pituitary dysfunction following traumatic brain injury in adults: British Neurotrauma Group guidance. J Neurol Neurosurg Psychiatry 88(11):971–981. https://doi.org/10.1136/jnnp-2016-315500
Ghigo E, Masel B, Aimaretti G, Léon-Carrión J, Casanueva FF, Dominguez-Morales MR, Elovic E, Perrone K, Stalla G, Thompson C, Urban R (2005) Consensus guidelines on screening for hypopituitarism following traumatic brain injury. Brain Inj 19(9):711–724. https://doi.org/10.1080/02699050400025315
Seckl J, Dunger D (1989) Postoperative diabetes insipidus. BMJ 298(6665):2–3
Group M (2009) o.C.m.W.: VA/DoD Clinical Practice Guideline for Management of Concussion/Mild Traumatic Brain Injury. J Rehabil Res Dev 46(6):CP1–C68
Marshall LF, Marshall SB, Klauber MR, Van Berkum Clark M, Eisenberg H, Jane JA, Luerssen TG, Marmarou A, Foulkes MA (1992) The diagnosis of head injury requires a classification based on computed axial tomography. J Neurotrauma 9(Suppl 1):S287–S292
van der Eerden AW, Twickler MT, Sweep FC, Beems T, Hendricks HT, Hermus AR, Vos PE (2010) Should anterior pituitary function be tested during follow-up of all patients presenting at the emergency department because of traumatic brain injury? Eur J Endocrinol 162(1):19–28. https://doi.org/10.1530/EJE-09-0436
Glynn N, Agha A (2013) Which patient requires neuroendocrine assessment following traumatic brain injury, when and how? Clin Endocrinol (Oxf) 78(1):17–20. https://doi.org/10.1111/cen.12010
Agha A, Tomlinson JW, Clark PM, Holder G, Stewart PM (2006) The long-term predictive accuracy of the short synacthen (corticotropin) stimulation test for assessment of the hypothalamic-pituitary-adrenal axis. J Clin Endocrinol Metab 91(1):43–47. https://doi.org/10.1210/jc.2005-1131
Molitch ME, Clemmons DR, Malozowski S, Merriam GR, Vance ML, Society E (2011) Evaluation and treatment of adult growth hormone deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab 96(6):1587–1609. https://doi.org/10.1210/jc.2011-0179
Corneli G, Di Somma C, Baldelli R, Rovere S, Gasco V, Croce CG, Grottoli S, Maccario M, Colao A, Lombardi G, Ghigo E, Camanni F, Aimaretti G (2005) The cut-off limits of the GH response to GH-releasing hormone-arginine test related to body mass index. Eur J Endocrinol 153(2):257–264. https://doi.org/10.1530/eje.1.01967
Dichtel LE, Yuen KC, Bredella MA, Gerweck AV, Russell BM, Riccio AD, Gurel MH, Sluss PM, Biller BM, Miller KK (2014) Overweight/Obese adults with pituitary disorders require lower peak growth hormone cutoff values on glucagon stimulation testing to avoid overdiagnosis of growth hormone deficiency. J Clin Endocrinol Metab 99(12):4712–4719. https://doi.org/10.1210/jc.2014-2830
Hannon MJ, Finucane FM, Sherlock M, Agha A, Thompson CJ (2012) Clinical review: disorders of water homeostasis in neurosurgical patients. J Clin Endocrinol Metab 97(5):1423–1433. https://doi.org/10.1210/jc.2011-3201
Kozlowski Moreau O, Yollin E, Merlen E, Daveluy W, Rousseaux M (2012) Lasting pituitary hormone deficiency after traumatic brain injury. J Neurotrauma 29(1):81–89. https://doi.org/10.1089/neu.2011.2048
Krahulik D, Zapletalova J, Frysak Z, Vaverka M (2010) Dysfunction of hypothalamic-hypophysial axis after traumatic brain injury in adults. J Neurosurg 113(3):581–584. https://doi.org/10.3171/2009.10.JNS09930
Berg C, Oeffner A, Schumm-Draeger PM, Badorrek F, Brabant G, Gerbert B, Bornstein S, Zimmermann A, Weber M, Broecker-Preuss M, Mann K, Herrmann BL (2010) Prevalence of anterior pituitary dysfunction in patients following traumatic brain injury in a German multi-centre screening program. Exp Clin Endocrinol Diabetes 118(2):139–144. https://doi.org/10.1055/s-0029-1225611
Kleindienst A, Brabant G, Bock C, Maser-Gluth C, Buchfelder M (2009) Neuroendocrine function following traumatic brain injury and subsequent intensive care treatment: a prospective longitudinal evaluation. J Neurotrauma 26(9):1435–1446. https://doi.org/10.1089/neu.2008.0601
Leal-Cerro A, Flores JM, Rincon M, Murillo F, Pujol M, Garcia-Pesquera F, Dieguez C, Casanueva FF (2005) Prevalence of hypopituitarism and growth hormone deficiency in adults long-term after severe traumatic brain injury. Clin Endocrinol (Oxf) 62(5):525–532. https://doi.org/10.1111/j.1365-2265.2005.02250.x
Bondanelli M, De Marinis L, Ambrosio MR, Monesi M, Valle D, Zatelli MC, Fusco A, Bianchi A, Farneti M, degli Uberti EC (2004) Occurrence of pituitary dysfunction following traumatic brain injury. J Neurotrauma 21(6):685–696. https://doi.org/10.1089/0897715041269713
Popovic V, Pekic S, Pavlovic D, Maric N, Jasovic-Gasic M, Djurovic B, Medic-Stojanoska M, Zivkovic V, Stojanovic M, Doknic M, Milic N, Djurovic M, Dieguez C, Casanueva FF (2004) Hypopituitarism as a consequence of traumatic brain injury (TBI) and its possible relation with cognitive disabilities andmental distress. J Endocrinol Invest 27(11):1048–1054. https://doi.org/10.1007/BF03345308
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interests.
Rights and permissions
About this article
Cite this article
Glynn, N., Agha, A. The frequency and the diagnosis of pituitary dysfunction after traumatic brain injury. Pituitary 22, 249–260 (2019). https://doi.org/10.1007/s11102-019-00938-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11102-019-00938-y