Why Are Your Gut Microbes Different From Mine?
To find out, scientists collected poop from thousands of people—but they ended up with more questions than answers.
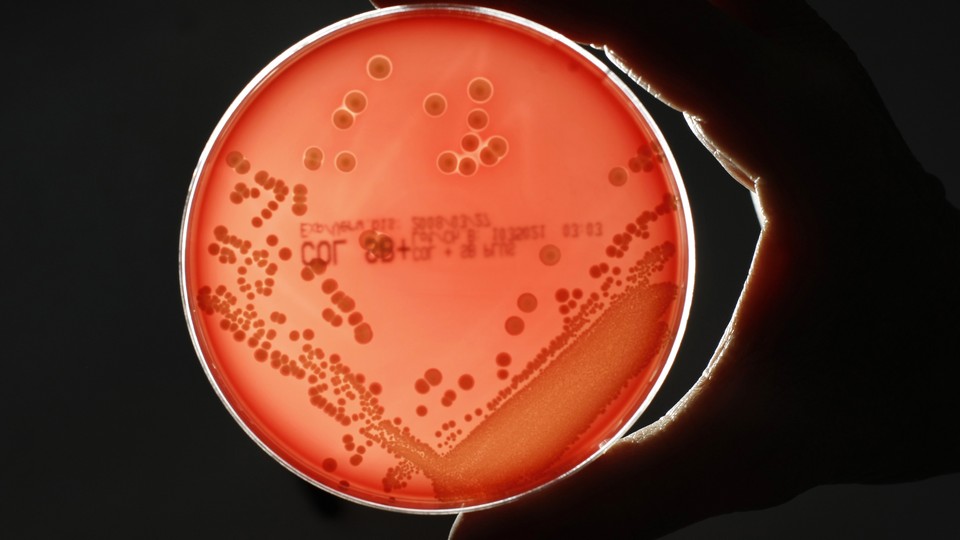
There are tens of trillions of bacteria in my gut and they are different from those in yours. Why?
This is a really basic question about the human microbiome and, rather vexingly, we still don’t have a good answer. Sure, we know some of the things that influence the roll call of species—diet and antibiotics, to name a few—but their relative importance is unclear and the list is far from complete. That bodes poorly for any attempt to work out whether these microbes are involved in diseases, and whether they can be tweaked to improve our health.
Two new studies have tried to address the problem. They’re the largest microbiome studies thus far published, looking at 1,135 Dutch adults and 1,106 Belgians respectively. Both looked at how hundreds of factors affect the microbiome, including age, height, weight, sleep, medical history, smoking, allergies, blood levels of various molecules, and a long list of foods. Both found dozens of factors that affect either the overall diversity of microbial species, or the abundance of particular ones. And encouragingly, their respective lists overlap considerably.
But here’s the important thing: Collectively, the factors they identified explain a tiny proportion of the variation between people’s microbiomes—19 percent in the Dutch study, and just 8 percent in the Belgian. Which means we’re still largely in the dark about what makes my microbiome different from yours, let alone whether one is healthier than the other.
“With all the knowledge we’ve gathered, we made the best possible effort to capture all the factors we could imagine, and we could only explain 8 percent of the total variation,” says Jeroen Raes from the University of Leuven, who led the Belgian study. “It’s very humbling.”
If this sounds familiar, it’s because geneticists went through a similar period of humility. Complex traits like height, intelligence, and schizophrenia risk are strongly heritable, but finding the genes that underlie them has been monstrously hard. Early on, researchers used small experiments to identify many genetic variants that are linked to diseases and physical traits. But later, larger studies revealed that many of these results were false alarms, prompting a move towards more rigorous methods.
The microbiome field is negotiating the same cycle of hype, backlash, and introspection. Thousands of studies have linked the microbiome to almost every condition you can imagine, but many of these correlations are likely to be illusory. “A lot of people have been annoyed by the hype surrounding our area, and I think they were probably right,” says Raes. “It’s time that, from within the field, we look critically at what we’re doing ourselves. We tried to do that with our paper. Yes, we’ve had the hype. Now, it’s time for the consolidation.”
Raes is right to be cautious. For example, his team found that the single thing that most strongly correlates with the make-up of the gut microbiome is the consistency of one’s stool. Virtually no clinical studies have measured or accounted for that. This means that in the past, when scientists found differences between the microbiomes of sick and healthy people, those differences might have had nothing to do with disease. Maybe the sick people just had runnier poop. “It’s a wake-up call for all of us to start taking these things into account,” says Raes.
Medications are also important, from obvious ones like antibiotics and laxatives, to less intuitive ones like antihistamines, antidepressants, and metformin, which is used to treat type 2 diabetes. “It’s one of those elephants in the room,” says Raes. “Everyone knew [that drugs are important] but no one controlled for them.”
Several factors predictably affect the microbiome, including weight, age, gender and consumption of several foods and nutrients, whether it's bread, fruit, soda, coffee, tea, red wine, or dietary fiber.
Others links were inexplicable. The Dutch team found that the levels of chromogranin A (CgA), a protein secreted by intestinal cells, is strongly linked to the levels of 61 common species of microbe. “We don’t have a good explanation for that, and we know relatively little about this protein,” says Alexandra Zhernakova, who led the study. Meanwhile, Raes found that some Lachnospiraceae bacteria are more common in people who like dark chocolate. (“We don’t understand it, but I think it’s hilarious that you do a Belgian study and one of the factors that comes out is chocolate,” he says.)
And some connections were baffling in their absence. Although many past studies have shown that C-section deliveries and bottle-feeding can change the microbiomes of babies, neither factor affected the communities of the Belgian adults. “That was a shocker,” says Raes. “I think these are effects that wear off over time, but I don’t think that they’re not important.”
Large studies like these are often billed as fishing expeditions, which consider so many correlations that they’re bound to pass off statistical flukes as real results. But Raes argues that his team took extreme care to weed out all but the strongest links. Better still, they cross-checked their results against the Dutch data, and confirmed over 90 percent of their findings. “That blew me away,” he says. This sort of validation is common in genetics, but “is rarely done in the microbiome field,” adds Pat Schloss from the University of Michigan. “It’s something the field needs to start doing as claims that the microbiome controls everything continue to grow.”
But what did the teams miss? What else could explain the differences between our microbiomes, if not the ones they considered?
Neither study looked at genetics, and we know that some genes can influence which bacteria a person harbors. Raes suspects that interactions between the microbes are important, so that what affects the presence of Microbe X is the presence of Microbes Y and Z, rather than anything to do with their host. Zhernakova notes that they only collected one stool sample from each volunteer, and such snapshots can’t capture the highly dynamic nature of the microbiome, which shifts between meals, hours, and months. “We need more longitudinal studies to see what is stable or not,” she says. And Schloss suggests that the makeup of the microbiome may largely be “the accumulation of coincidences.”
We haven’t even identified all the players yet. By combining data from the Dutch and Flemish studies with earlier British and American ones, Raes’s team identified a total number of 664 bacterial genera. But they estimate that at least 80 more haven’t been identified, and doing so will take studies that are ten times larger than the current record-holders. That’s a common theme throughout all of microbiology—the unknowns are vast. “Even though we’re the biggest study out there, we’re still scratching the surface when it comes to charting the whole microbiota population,” says Raes. “We should be humble.”