 Efficient, low-cost, field-ready functional movement tests may be useful in preparticipation physicals to identify and provide preventive treatment for individuals with an elevated risk of injury, as well as aiding return-to-sport decisions when used at discharge from rehabilitation.
Efficient, low-cost, field-ready functional movement tests may be useful in preparticipation physicals to identify and provide preventive treatment for individuals with an elevated risk of injury, as well as aiding return-to-sport decisions when used at discharge from rehabilitation.
By Kathryn Schwartzkopf-Phifer, PT, DPT, OCS, CSCS, and Kyle Kiesel, PT, PhD, ATC
It is well known that the most common sports injuries occur in the lower extremity, most notably the ankle, knee, and hamstring.1-3 Researchers have identified multiple risk factors associated with athletic injury in efforts to reduce injury rates, the associated disability, and healthcare costs.4 The majority of research to date has focused on individual risk factors associated with specific injuries while controlling for the most common and strongest risk factor, previous injury.
Although previous injury in and of itself is not modifiable,5-8 many of the residual effects of injury, such as changes in motor control,9,10-13 are. For example, researchers have observed delays in the activation of the hip musculature in patients with a history of ankle instability.10,11,13 These subtle changes in motor control at the hip, regardless of the status of the ankle, may be a contributing factor for subsequent injury. Additionally, Cholewicki et al have shown that excessive outer core-muscle activation patterns are present in athletes with a history of low back pain, even though they were pain free at the time they were tested.14,15
These excessive activation patterns resulted in fewer outer core muscles being shut off after a response to a sudden load, with athletes with a history of low back pain shutting muscles off more slowly than those without a history of low back pain. These altered core activation strategies are also related to subsequent knee ligamentous injury.16 Taken collectively, these data suggest that an alteration in the timing and coordination of core and hip muscles exists in athletes following lower extremity injury and may be worthy of consideration when screening for future injury risk.
It is challenging to efficiently screen or test for core and hip motor control dysfunction, as this involves time-consuming and highly technical lab testing. Therefore, it may be desirable to perform alternate tests of fundamental movement that assess how the individual coordinates and controls his or her own body weight. Measurement of performance on such basic tasks involving a single body-weight movement may provide a better understanding of an athlete’s intrinsic motor control that may have been compromised by previous injury.
Such basic movement tests could provide insight into injury risk and serve as standardized assessments practitioners could perform when patients are discharged from rehabilitation in an effort to reduce the effects of previous injury on injury risk.17
The FMS and Y-balance test
Researchers have identified two reliable field-expedient measures involving motor control of body-weight movement tasks that have been associated with identifying athletes at increased risk of injury. While the majority of athletes who demonstrate dysfunction on these basic body-weight tests do have a history of injury, the tests are also useful for identifying those with poor underlying fundamental movement regardless of injury history. We speculate that improper strength and conditioning practices may be related to the development of dysfunctional movement.
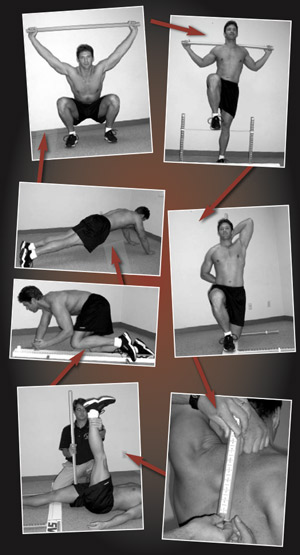
Research has shown that the Functional Movement Screen (FMS) (Figure 1) has acceptable to excellent reliability18-24 and that clinicians can use it efficiently in a mass screening environment.25 The FMS ranks seven fundamental movement patterns, incorporates three clearing tests, and is designed to screen for major movement limitations and asymmetries26,27 (see Table 1).
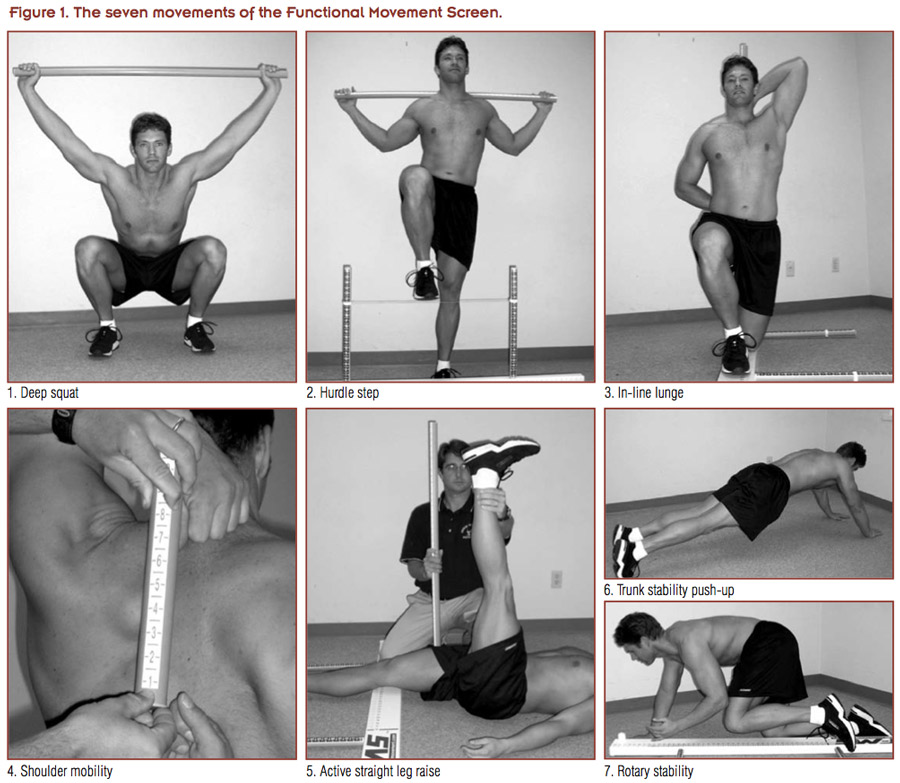 Several injury risk studies have established predictive validity of the FMS. A composite score of less than or equal to 14 on the FMS, for example, is predictive of injury in professional football players,28,29 female collegiate athletes,30 firefighters,31 and military personnel.32,33 The presence of any asymmetrical movement is related to increased injury risk in professional football players.29
Several injury risk studies have established predictive validity of the FMS. A composite score of less than or equal to 14 on the FMS, for example, is predictive of injury in professional football players,28,29 female collegiate athletes,30 firefighters,31 and military personnel.32,33 The presence of any asymmetrical movement is related to increased injury risk in professional football players.29
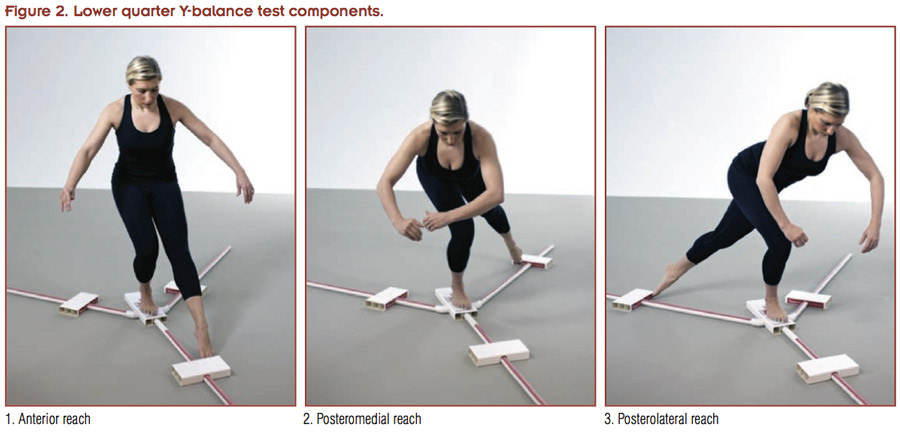
Another reliable motor control test is the lower quarter Y-balance test (YBT-LQ)34,35 (Figure 2). The YBT-LQ requires single-limb dynamic balance while the contralateral limb completes an open chain excursion in the anterior, posteromedial, and posterolateral directions. The greatest reach is normalized to limb length, and testers also report each of the three directions on the right and left sides as well as right and left composite scores. This provides an objective measure of how individuals perform near their limits of stability.
 Research has shown that performance on the YBT-LQ is related to injury risk in several populations, including female high school basketball players, in whom symmetry and scoring poorly compared with age-matched norms increased the likelihood of injury.34 Poor performance has also been found to be predictive of ankle sprains in college-aged individuals,36 and researchers have reported that poor performance has a relationship with lower extremity injury risk in college football players.37 Investigators have published a systematic review of YBT-LQ research.38
Research has shown that performance on the YBT-LQ is related to injury risk in several populations, including female high school basketball players, in whom symmetry and scoring poorly compared with age-matched norms increased the likelihood of injury.34 Poor performance has also been found to be predictive of ankle sprains in college-aged individuals,36 and researchers have reported that poor performance has a relationship with lower extremity injury risk in college football players.37 Investigators have published a systematic review of YBT-LQ research.38
Because of the wide variety of known risk factors for lower extremity injury, and because most studies examine only a single diagnosis (such as an anterior cruciate ligament [ACL] tear) and frequently require lab-based testing, it previously has been challenging to determine injury risk using field-based screening and testing. An option proposed in the literature39 involves synthesizing multiple evidence-based factors and using an algorithmic approach to categorize an individual’s risk. For example, if an athlete presents with multiple known risk factors, such as recent injury, poor movement, and asymmetrical movement, that athlete would be categorized as being at greater risk than an athlete demonstrating just one of those factors. Each factor can also be weighted based on the strength of evidence from the current literature regarding that factor.
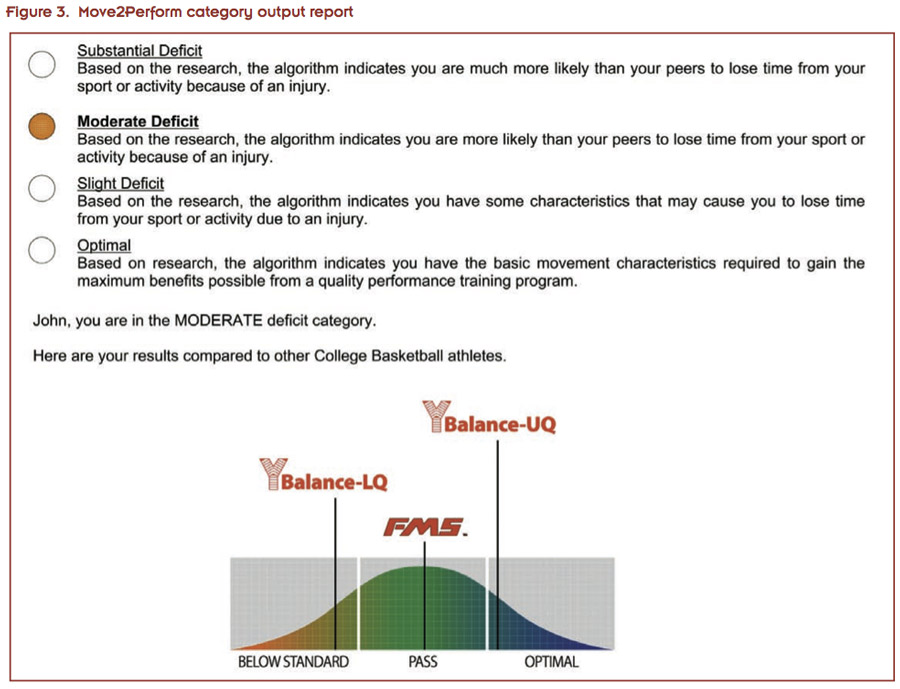
This approach was developed by researchers and tested in a 2013 study of collegiate athletes.39 The study examined the relationship between the risk category calculated by the Move2Perform injury risk algorithm and noncontact lower extremity time-loss injury. The algorithm weights a variety of evidenced-based factors that can be collected in an efficient manner in a standard preparticipation physical mass screening setting, including FMS score and asymmetry, YBT-LQ performance, injury history, current pain, gender, and sport.
The computerized algorithm places each individual into one of four risk categories that include Substantial and Moderate (considered “high risk”) and Slight and Normal (considered “low risk”). The study demonstrated that athletes placed in the high-risk group had a relative risk (RR) of 3.4 (95% CI: 2.0 to 6.0), indicating they were 3.4 times more likely to be injured over the course of their respective sport seasons than those in the low-risk group.
 Although poor performance on the FMS and YBT-LQ are predictive of injury, evidence suggests these risk factors are also modifiable. Investigators collected FMS scores for 62 professional football players prior to their beginning a supervised off-season strength and conditioning program.40 They prescribed athletes individualized exercise programs designed to address their specific movement deficits or asymmetries based on their FMS results. Exercises included self and partner stretching, treatment of trigger points, and “corrective exercises,” which emphasized use of the improved mobility as well as appropriate core activation. Athletes did these exercises for seven weeks and investigators then repeated FMS testing. Of the 55 athletes who scored 14 or lower on the composite threshold at pretesting, 32 improved their scores to more than 14 after the intervention period. Forty two athletes were free of asymmetry at post-test, compared with 31 at pretest.
Although poor performance on the FMS and YBT-LQ are predictive of injury, evidence suggests these risk factors are also modifiable. Investigators collected FMS scores for 62 professional football players prior to their beginning a supervised off-season strength and conditioning program.40 They prescribed athletes individualized exercise programs designed to address their specific movement deficits or asymmetries based on their FMS results. Exercises included self and partner stretching, treatment of trigger points, and “corrective exercises,” which emphasized use of the improved mobility as well as appropriate core activation. Athletes did these exercises for seven weeks and investigators then repeated FMS testing. Of the 55 athletes who scored 14 or lower on the composite threshold at pretesting, 32 improved their scores to more than 14 after the intervention period. Forty two athletes were free of asymmetry at post-test, compared with 31 at pretest.
Significant improvements in FMS scores also have been demonstrated in other active populations. After completing six weeks of a yoga-based program, mean FMS scores improved from 13.25 to 16.55 in a sample of firefighters, who were more likely to be injured during training if their FMS score was less than or equal to 14.41 An average FMS score improvement of 2.5 points was also noted in special operations soldiers following a six-week functional training program that focused on improving agility, core strength, balance, and power.42
A randomized controlled trial by Bodden et al demonstrated a significant change in the number of athletes scoring above the threshold of 14, as well as the number of athletes with any asymmetry on the FMS following a four-week individualized exercise program in mixed martial arts.43
A multimodal training approach has also been effective for improving dynamic balance in female youth soccer players as measured by the star excursion balance test (SEBT), a motor control test similar to the YBT-LQ. Athletes did an injury prevention program (FIFA 11+), which consisted of agility training, strengthening, plyometrics, balance exercises, and running, approximately two times per week for seven to 11 weeks. Although all athletes experienced an improvement in SEBT scores, those athletes who were highly adherent to the program had a 72% lower injury risk than those who were less adherent.44 Athletes also performed exercises under three different conditions. A control group received access to the FIFA 11+ website only, while another group received an instructional workshop for the program in addition to website access. The final group received the instructional workshop, website access, plus contact with a physiotherapist who attended weekly sessions to assist with appropriate technique and exercise progression. Significantly greater improvement was noted in the physiotherapist- assigned group than the control group, particularly in the anterior reach direction of the SEBT.
 It should be noted that previous research has emphasized the importance of the anterior reach in injury prediction.34 Therefore, a multimodal training program was not only effective at improving scores on the SEBT, but this improvement also led to decreased injury risk.
It should be noted that previous research has emphasized the importance of the anterior reach in injury prediction.34 Therefore, a multimodal training program was not only effective at improving scores on the SEBT, but this improvement also led to decreased injury risk.
A pilot study45 has also demonstrated that an intervention program can change an athlete’s injury risk category. Using the algorithm approach described previously, Huebner et al45 reported a significant number of high school female soccer players changed from higher to lower risk categories following an eight-week supervised intervention program that included individual movement correction exercises and a group jump training program.
Collectively, the results of these studies indicate that, through a variety of intervention strategies, athletes can improve FMS score and YBT performance, and potentially reduce their injury risk.
A recent study has also suggested a relationship exists between FMS scores and performance.46 Chapman et al collected FMS scores on 121 elite track and field athletes and compared their best performance between two consecutive seasons. Athletes scoring greater than 14 on the FMS had a significantly different change in performance (+.41 ± 2.5%) between seasons compared with those scoring 14 or less (–.51 ± 2.3%). Performance changes for athletes demonstrating at least one asymmetry on any of the bilateral movements was –.26 ± 2.1% compared with +.60 ± 2.86% for athletes without asymmetry. Additionally, athletes scoring a three on the deep squat had a significantly greater improvement in performance compared with those scoring one or two. This is an interesting finding, as previous research isolating deep squat scores demonstrates that athletes were nearly five times more likely to fail to improve total FMS scores if they scored a one on the deep squat. While total FMS score, and even individual components of the FMS, have been predictive of injury and improvement potential, there is some evidence that its use can be extended to predict performance as well.
Clinical application
Injuries come at a cost, not only to athletes and their families, but also to the schools, universities, or organizations for which they play. If athletes at high risk for injury can be identified during a preseason screen, appropriate interventions can be implemented and the financial burden of these injuries can be avoided. The FMS and the YBT-LQ are field-expedient, reliable tools that can be combined with demographic information to predict lower extremity injuries in active populations.
Athletes can then be placed into categories of injury risk based on the presence of known evidence-based risk factors. Identification of high-risk athletes can have time and cost-saving benefits by allowing clinicians to focus preventive efforts on those who need it most. High-risk athletes can receive one-on-one care from clinicians, addressing specific areas of deficit to improve performance in fundamental movements and dynamic stability. Ultimately, these improvements lead to a change in category of risk and limit the effects of the previously named risk factors. Once a lower injury risk category is achieved, these athletes can receive instruction in a generalized preventive program, along with other low-risk athletes, with minimal supervision to improve performance and decrease injury risk. Coaching staff can implement and monitor these preventive programs, thereby reducing demands on clinical staff.
These tests are advantageous, not only because of the information to be gained, but also because they are quickly administered and easily used and interpreted by medical and coaching personnel (Figure 3). Staff and funding are limited at many institutions and under these circumstances, these tests can facilitate evidence-based, cost-effective allocation of resources.
Conclusion
Lower extremity injuries are common in sports, and the strongest risk factor associated with these injuries is previous injury. Because of the well-known motor control changes that occur with injury, basic single body-weight, movement-oriented testing may be helpful in determining how previous injury has affected the motor control of basic body-weight movement tasks. An injury prediction algorithm has been proposed that utilizes efficient, low-cost, field-ready tests and brief historic injury data to categorize an athlete’s injury risk. The initial research on this algorithm is promising, and further research is warranted. Ultimately, the tests used with the injury prediction algorithm may be useful in preparticipation physicals to identify individuals with an elevated risk of injury and to aid return-to-sport decisions when used at discharge from rehabilitation.
Kathryn Schwartzkopf-Phifer, PT, DPT, OCS, CSCS, is an instructor in the Department of Physical Therapy at the University of Evansville, IN, and a doctoral student in the Rehabilitation Sciences Program at the University of Kentucky in Lexington. Kyle Kiesel, PT, PhD, ATC, is a professor of physical therapy at the University of Evansville.
- Elliott MC, Zarins B, Powell JW, Kenyon CD. Hamstring muscle strains in professional football players: a 10-year review. Am J Sports Med2011;39(4):843-850.
- Shah VM, Andrews JR, Fleisig GS, et al. Return to play after anterior cruciate ligament reconstruction in National Football League athletes. Am J Sports Med 2010;38(11):2233-2239.
- Hootman JM, Dick R, Agel J. Epidemiology of collegiate injuries for 15 sports: summary and recommendations for injury prevention initiatives. J Athl Train2007;42(2):311-319.
- Dick R, Agel J, Marshall SW. National Collegiate Athletic Association Injury Surveillance System commentaries: introduction and methods. J Athl Train 2009;44(2):173-182.
- Emery CA. Identifying risk factors for hamstring and groin injuries in sport: a daunting task. Clin J Sport Med 2012;22(1):75-77.
- Engebretsen AH, Myklebust G, Holme I, et al. Intrinsic risk factors for groin injuries among male soccer players: a prospective cohort study. Am J Sports Med 2010;38(10):2051-2057.
- Engebretsen AH, Myklebust G, Holme I, et al. Intrinsic risk factors for hamstring injuries among male soccer players: a prospective cohort study. Am J Sports Med 2010;38(6):1147-1153.
- Engebretsen AH, Myklebust G, Holme I, et al. Intrinsic risk factors for acute ankle injuries among male soccer players: a prospective cohort study. Scand J Med Sci Sports 2010;20(3):403-410.
- Opar DA, Williams MD, Shield AJ. Hamstring strain injuries: factors that lead to injury and re-injury. Sports Med 2012;42(3):209-226.
- Beckman SM, Buchanan TS. Ankle inversion injury and hypermobility: effect on hip and ankle muscle electromyography onset latency. Arch Phys Med Rehabil 1995;76(12):1138-1143.
- Bullock-Saxton JE, Janda V, Bullock MI. The influence of ankle sprain injury on muscle activation during hip extension. Int J Sports Med 1994;15(6):330-334.
- Zazulak BT, Hewett TE, Reeves NP, et al. The effects of core proprioception on knee injury: a prospective biomechanical-epidemiological study. Am J Sports Med 2007;35(3):368-373.
- Van Deun S, Staes FF, Stappaerts KH, et al. Relationship of chronic ankle instability to muscle activation patterns during the transition from double-leg to single-leg stance. Am J Sports Med 2007;35(2):274-281.
- Cholewicki J, Greene HS, Polzhofer GK, et al. Neuromuscular function in athletes following recovery from a recent acute low back injury. J Orthop Sports Phys Ther 2002;32(11):568-575.
- Cholewicki J, Silfies SP, Shah RA, et al. Delayed trunk muscle reflex responses increase the risk of low back injuries. Spine 2005;30(23):2614-2620.
- Zazulak BT, Hewett TE, Reeves NP, et al. Deficits in neuromuscular control of the trunk predict knee injury risk: a prospective biomechanical-epidemiologic study. Am J Sports Med 2007;35(7):1123-1130.
- Kiesel KB, Plisky PJ. Establishing functional baselines and appropriate training for off-season conditioning and injury prevention; Best Practices in Functional Testing in Sports. In: Liebenson C, ed. The Functional Training Handbook. Philadelphia, PA: Lippincott Williams & Wilkins; 2014.
- Frohm A, Heijne A, Kowalski J, et al. A nine-test screening battery for athletes: a reliability study. Scand J Med Sci Sports2012;22(3):306-315.
- Gribble PA, Brigle J, Pietrosimone BG, et al. Intrarater reliability of the functional movement screen. J Strength Cond Res 2013;27(4):978-981.
- Minick KI, Kiesel KB, Burton L, et al. Interrater reliability of the functional movement screen. J Strength Cond Res 2010;24(2):479-486.
- Onate JA, Dewey T, Kollock RO, et al. Real-time intersession and interrater reliability of the functional movement screen. J Strength Cond Res 2012;26(2):408-415.
- Gulgin H,Hoogenboom B. The functional movement screening (FMS)™: an inter-rater reliability study between raters of varied experience. Int J Sports Phys Ther2014;9(1):14-20.
- Smith C, Chimera N, Wright N, Warren M. Interrater and intrarater reliability of hte functional movement screen. J Strength Cond Res2013;27(4):982-987.
- Teyhen DS, Shaffer SW, Lorenson CL, et al. The functional movement screen: a reliability study. J Orthop Sports Phys Ther2012;42(6):530-540.
- Teyhen DS, Shaffer SW, Umlauf JA, et al. Automation to improve efficiency of field expedient injury prediction screening. J Strength Cond Res 2012;26 Suppl 2:S61-72.
- Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function – part 2. N Am J Sports Phys Ther 2006;1(3):132-139.
- Cook G, Burton L, Hoogenboom B. Pre-participation screening: the use of fundamental movements as an assessment of function – part 1. N Am J Sports Phys Ther 2006;1(2):62-72.
- Kiesel K, Plisky PJ, Voight ML. Can serious injury in professional football be predicted by a preseason functional movement screen? N Am J Sports Phys Ther 2007;2(3):147-158.
- Kiesel KB, Butler RJ, Plisky PJ. Limited and asymmetrical fundamental movement patterns predict injury in american football players. J Sport Rehabil 2014;23(2):88-94.
- Chorba RS, Chorba DJ, Bouillon LE, et al. Use of a functional movement screening tool to determine injury risk in female collegiate athletes. N Am J Sports Phys Ther 2010;5(2):47-54.
- Butler RJ, Contreras M, Burton L, et al. Modifiable risk factors predict injuries in firefighter during training academies. Work2013;46(1):11-17.
- Lisman P, O’Connor FG, Deuster PA, Knapik JJ. Functional movement screen and aerobic fitness predict injuries in military training. Med Sci Sports Exerc 2013;45(4):636-643.
- O’Connor FG, Deuster PA, Davis J, et al. Functional movement screening:predicting injuries in officer candidates. Med Sci Sports Exerc2011;43(12):2224-2230.
- Plisky PJ, Rauh MJ, Kaminski TW, Underwood FB. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J Orthop Sports Phys Ther2006;36(12):911-919.
- Plisky PJ, Gorman PP, Butler RJ, et al. The reliability of an instrumented device for measuring components of the star excursion balance test. N Am J Sports Phys Ther 2009;4(2):92-99.
- de Noronha M, Franca LC, Haupenthal A, Nunes GS. Intrinsic predictive factors for ankle sprain in active university students: A prospective study. Scand J Med Sci Sports 2013;23(5):541-547.
- Butler RJ, Lehr ME, Fink ML, et al. Dynamic balance performance and noncontact lower extremity injury in college football players: an initial study. Sports Health 2013;5(5):417-422.
- Gribble PA, Hertel J, Plisky P. Using the Star Excursion Balance Test to assess dynamic postural-control deficits and outcomes in lower extremity injury: a literature and systematic review. J Athl Train 2012;47(3):339-357.
- Lehr ME, Plisky PJ, Butler RJ, et al. Field-expedient screening and injury risk algorithm categories as predictors of noncontact lower extremity injury. Scand J Med Sci Sports2013;23(4):e225-e232
- Kiesel K, Plisky P, Butler R. Functional movement test scores improve following a standardized off-season intervention program in professional football players. Scand J Med Sci Sports2011;21(2):287-292.
- Cowen VS. Functional fitness improvements after a worksite-based yoga initiative. J Bodyw Mov Ther 2010;14(1):50-54.
- Goss DL, Christopher GE, Faulk RT, Moore J. Functional training program bridges rehabilitation and return to duty. J Spec Oper Med 2009 Spring;9(2):29-48.
- Bodden JG, Needham RA, Chockalingam N. The effect of an intervention program on functional movement screen test scores in mixed martial arts athletes. J Strength Cond ResJul 15 2013. [Epub ahead of print]
- Steffen K, Emery CA, Romiti M, et al. High adherence to a neuromuscular injury prevention programme (FIFA 11+) improves functional balance and reduces injury risk in Canadian youth female football players: a cluster randomised trial. Br J Sports Med 2013;47(12):794-802.
- Heubner B, Riley M, Alm A, Matsell K. A pre-season injury prevention training program improves movement test scores and injury risk category. Paper presented at the 60th Annual American College of Sports Medicine Annual Meeting and 3rd World Congress on Exercise is Medicine, Indianapolis, IN, June, 2012.
- Chapman RF, Laymon AS, Arnold T. Functional movement scores and longitudinal performance outcomes in elite track and field athletes. Int J Sports Physiol Perform 2014;9(2):203-211.